2006
Feasibility of Post-Gadolinium T1 SPACE Brain Imaging at 7T
Eric G. Stinson1,2, Peter Kollasch1,2, John Lane2, Kirk Welker2, and Andrew J. Fagan2
1Siemens Medical Solutions USA, Inc., Rochester, MN, United States, 2Radiology, Mayo Clinic, Rochester, MN, United States
1Siemens Medical Solutions USA, Inc., Rochester, MN, United States, 2Radiology, Mayo Clinic, Rochester, MN, United States
Synopsis
Post-contrast imaging is useful for visualizing enhancing lesions, but when using MPRAGE at 7T the high vascular signal, gray/white matter contrast, and susceptibility-induced artifacts can confound visualization of enhancing lesions. T1-weighted SPACE imaging has been shown to provide improved visualization at 3T, but has not been used at 7T. Here, we show improved visualization of enhancing lesions at 7T with a T1 SPACE technique that avoids the downsides of post-Gadolinium MPRAGE imaging.
Introduction
MPRAGE (1) is commonly used for both pre- and post-contrast imaging to depict the structural anatomy of the brain. While it can provide high resolution, high SNR, and excellent gray/white matter contrast, it does suffer from some downsides for post-contrast imaging. First, the vascular signal is high and can confound visualization of small enhancing lesions. Second, MPRAGE is sensitive to the susceptibility-induced effects of Gadolinium-based contrast agent in the blood, and suffers from signal loss and image distortion as a result. Third, the gray/white matter contrast that is an advantage in pre-contrast images is not always desirable when determining the margins of an enhancing lesion against the brain matter.T1-weighted 3D fast spin echo imaging with a variable-flip-angle schedule (T1 SPACE; T1-weighted Sampling Perfection with Application optimized Contrasts using different flip angle Evolution) (2-3) has been reported to overcome many of these problems at 3T and allow for better post-contrast visualization of metastatic tumors (4). To our knowledge, post-contrast T1-SPACE imaging at 7T has not yet been reported. The purpose of this work is to report on the feasibility of T1-weighted SPACE imaging for post-contrast brain imaging at 7T and compare to MPRAGE imaging results.
Methods
Imaging was performed on a MAGNETOM Terra 7T system (Siemens Healthcare, Erlangen, Germany) at software version VE12U. All imaging utilized product sequences and was performed with approval from the local institutional review board. Post-contrast imaging was performed in patients (n=3) to assess the utility of both MPRAGE and T1 SPACE for depicting enhancing brain lesions. Because the concentration of Gadolinium in the blood can affect the level of susceptibility-induced artifacts and changes over time after injection, the order of acquisition after contrast injection was varied, with MPRAGE performed first for some patients and second for other. Typical imaging parameters are shown in Table 1.Results
All imaging was performed successfully. In Figures 1-3, window width and window level were chosen to optimally display the enhancing pathology and were kept constant within each figure. Image results from a patient with a meningioma in the right frontal lobe are shown in Figure 1. In this case, the MPRAGE scan was performed first. Note the improved delineation of the tumor margin on the T1 SPACE images compared to the MPRAGE images. Additionally, the vascular signal is reduced and the susceptibility-induced artifacts are eliminated.Figure 2 shows images from a patient with a cavernous malformation in the right temporal lobe. In this case, the MPRAGE scan was again performed first. Again, the susceptibility-induced artifacts are reduced and the margins of the malformation are better delineated against the flat gray/white matter contrast in the T1 SPACE. Also of note, the vascular signal in the brain is reduced in the T1 SPACE, making the enhancing malformation more conspicuous.
Images of a midbrain cavernous malformation are shown in Figure 3. In this case, the T1 SPACE was acquired immediately after contrast injection, unlike the other two examples shown in this abstract. Despite the difference in the acquisition order, the T1 SPACE images still show reduced vascular signal, improved margins, and excellent depiction of the internal structure of the malformation.
Discussion
Post-contrast T1 SPACE imaging has a number of advantages over MPRAGE, including reduced vascular signal, a flatter gray/white matter contrast as background for enhancing lesions, and fewer susceptibility-induced artifacts. One disadvantage of using T1 SPACE is reduced signal in the base of the brain and brain stem. This is due to the effect of B1 inhomogeneity that is compounded in T1 SPACE compared to MPRAGE due to the greater number of RF pulses per TR and the higher flip angles of those RF pulses. Nonetheless, the MR signal at the base of the brain appears to be adequate in both sequences, and with the additional vascular suppression offered by the T1 SPACE sequence, enhancing lesions may be visualized in spite of the overall signal loss. This hypothesis will be tested in the future as more patients are recruited.This study does have some limitations. First, we have yet to encounter any patients with small metastases, so a primary use case of this technique has not yet been tested. Second, the order of acquisition after contrast injection can affect the concentration of Gadolinium in the blood, and thus affect the susceptibility-induced artifacts. As illustrated in Figure 3, order randomization is currently being performed, but more examples are needed to draw a conclusion about the effect it may have on image quality. Third, no radiological evaluation has been performed at this time to determine if the advantages of T1 SPACE will translate to improved diagnosis. Future work will address these limitations through additional patient recruitment and a radiological evaluation.
Conclusion
An optimized T1 SPACE protocol was developed for post-contrast imaging at 7T and compared to the MPRAGE currently used at our institution. T1 SPACE with the parameters described in this work has the advantages of reduced vascular signal, flatter gray/white matter contrast, and reduced susceptibility-induced artifacts compared to MPRAGE post-contrast imaging.Acknowledgements
No acknowledgement found.References
- Mugler JP, Brookeman JR. Three-dimensional magnetization-prepared rapid gradient-echo imaging (3D MP RAGE). Magn. Reson. Med. 1990;15:152–157 doi: 10.1002/mrm.1910150117.
- Mugler JP, Bao S, Mulkern RV, et al. Optimized Single-Slab Three-dimensional Spin-Echo MR Imaging of the Brain. Radiology 2000;216:891–899 doi: 10.1148/radiology.216.3.r00au46891.
- Mugler JP. Optimized three-dimensional fast-spin-echo MRI: Optimized 3D Fast-Spin-Echo MRI. Journal of Magnetic Resonance Imaging 2014;39:745–767 doi: 10.1002/jmri.24542.
- Reichert M, Morelli J, Runge V, et al. Contrast-Enhanced 3-Dimensional SPACE Versus MP-RAGE for the Detection of Brain Metastases: Considerations With a 32-Channel Head Coil. Investigative Radiology 2013;48:55–60 doi: 10.1097/RLI.0b013e318277b1aa.
Figures
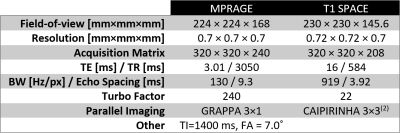
Table 1: Typical scan parameters for post-Gadolinium imaging
of the brain used in this study.
Field-of-view, Acquisition Matrix, and Resolution are presented in freq.
×
phase × slice order, or SI × AP × LR for these sagittal acquisitions.
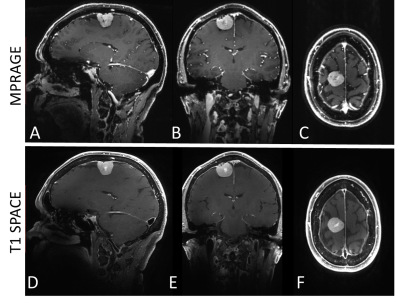
Figure 1: Post-Gadolinium
imaging of a meningioma using MPRAGE and T1 SPACE at 7T. In this case, the MPRAGE was acquired first
and the T1 SPACE was acquired immediately after. Note the reduced
susceptibility-induced artifacts in the T1 SPACE image, allowing for excellent
visualization of the tumor structure and margin. Additionally, the reduced vascular signal in
the T1 SPACE imaging allows for more conspicuous tumor enhancement.
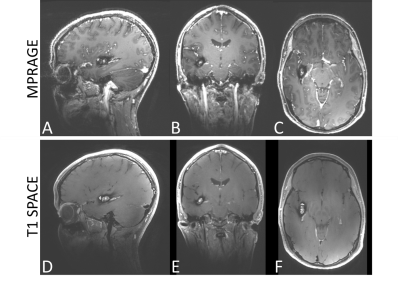
Figure 2: A cavernous
malformation imaged post-contrast using MPRAGE and T1 SPACE at 7T. In this case, the MPRAGE was acquired first
and the T1 SPACE was acquired immediately after. Here, the reduced vascular
signal in the T1 SPACE imaging allows for clearer differentiation between the
malformation and the surrounding normal vasculature.
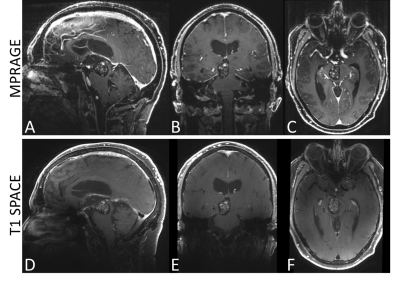
Figure 3: In this
example of post-Gadolinium imaging of a cavernous malformation in the midbrain,
the T1 SPACE was acquired first – in contrast to the other examples shown in
this work. Note the reduced susceptibility-induced artifacts in the T1 SPACE
image, allowing for excellent visualization of the internal structure and
margin. Again, the reduced vascular
signal in the T1 SPACE imaging allows for differentiation between the
malformation and the surrounding normal vasculature.