1993
Common and distinct patterns of intrinsic brain activity alterations in major depression and bipolar disorder: voxel-based meta-analysis1Medical Imaging Center, First Affiliated Hospital of Jinan University, Guangzhou, China, 2Department of Radiology, Six Affiliated Hospital of Sun Yat-sen University, Guangzhou, China, 3Department of Applied Psychology, Guangdong University of Foreign Studies, Guangzhou, China, 4MR Research, GE Healthcare, Beijing, China
Synopsis
This is the largest voxel-based meta-analysis conducted to date of amplitude of low-frequency fluctuation (ALFF) studies in major depressive disorder (MDD) and bipolar disorder (BD). MDD and BD show a common pattern of aberrant regional intrinsic brain activity which predominantly includes the insula, medial prefrontal cortex (mPFC), and cerebellum. These results expand on a growing literature exploring resting-state activity in MDD and BD, which provide useful insights for understanding the underlying pathophysiology of brain dysfunction in affective disorders, and developing more targeted and efficacious treatment and intervention strategies.
Introduction
Affective disorders, such as MDD (or unipolar depression) and BD, are highly prevalent and debilitating conditions associated with high suicide rates and a heavy social burden.1,2 Neuroimaging evidence has identified brain structural and functional alterations in multiple neuronal circuits in both MDD and BD.3-4 Identification of intrinsic brain activity differences and similarities between MDD and BD is a necessary step to better understand the underlying brain abnormalities in affective disorders and target more effective treatments. However, results have not yet yielded been consistent.Methods
A meta-analysis of whole-brain resting-state functional MRI (rs-fMRI) studies that explored differences in the ALFF between patients (including MDD and BD) and healthy controls (HCs) were conducted using the signed differential mapping (SDM) software package, a well-established and validated meta-analytic tool for neuroimaging studies that has been widely used to detect the most spatially consistent structural and functional brain changes in a number of neuropsychiatric diseases.Results
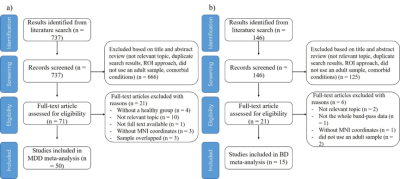
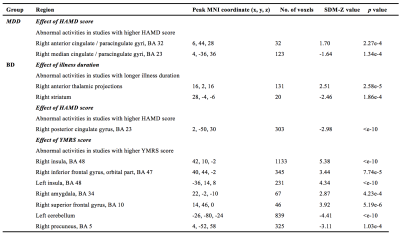
Systematic literature search identified 50 studies comparing 1399 MDD patients and 1332 HCs, 15 studies comparing 494 BD patients and 593 HCs. A flow diagram of the identification and exclusion of studies is presented in Fig. 1. As illustrated in Fig. 2, MDD patients displayed increased ALFF in the right superior frontal gyrus (SFG) (including the medial orbitofrontal cortex, mPFC, and anterior cingulate cortex (ACC)), bilateral insula and decreased ALFF in the bilateral cerebellum, bilateral precuneus, and left occipital cortex compared with HCs. BD patients showed increased ALFF in the bilateral inferior frontal gyrus (IFG), bilateral insula, right SFG, and right superior temporal gyrus (STG) and decreased ALFF in the left cerebellum, bilateral precuneus, left ACC, and left STG. In addition, MDD displayed increased ALFF in the left lingual gyrus, left ACC, bilateral precuneus/posterior cingulate gyrus (PCC), and left STG and decreased ALFF in the right insula, right mPFC, right fusiform gyrus, and bilateral striatum relative to BD patients. Conjunction analysis showed increased ALFF in the bilateral insula, mPFC, and decreased ALFF in the left cerebellum in both disorders. In patients with MDD, meta-regression analysis indicated that higher HAMD score was correlated with greater increases in ALFF in the right ACC. In patients with BD, meta-regression analysis revealed that higher HAMD score exhibited lesser decreases in ALFF in the right PCC. Mean illness duration was not associated with any MDD-related ALFF changes. The results of the meta-regression analyses are presented in Table 1.Discussion and Conclusion
In this paper, we report findings from the largest voxel-based meta-analysis conducted to date of ALFF studies in MDD and BD. We compared results to identify both common and different patterns of spontaneous brain activity alterations. Our comprehensive meta-analysis suggests that MDD and BD show a common pattern of aberrant regional intrinsic brain activity which predominantly includes the insula, mPFC, and cerebellum, while the limbic system may be associated with spatially distinct patterns of brain function, which provide useful insights for understanding the underlying pathophysiology of brain dysfunction in affective disorders, and developing more targeted and efficacious treatment and intervention strategies.Acknowledgements
No acknowledgement found.References
1. Grande I, Berk M, Birmaher B, Vieta E. Bipolar disorder. The Lancet. 2016; 387(10027): 1561-72.
2. Hirschfeld R, Lewis L, Vornik LA. Perceptions and impact of bipolar disorder: how far have we really come? results of the National Depressive and Manic-Depressive Association 2000 survey of individuals with bipolar disorder. The Journal of clinical psychiatry. 2003 Feb.
3. Han KM, De Berardis D, Fornaro M, Kim YK. Differentiating between bipolar and unipolar depression in functional and structural MRI studies. Progress in Neuro-Psychopharmacology and Biological Psychiatry. 2019; 91:20-7.
4. Niu M, Wang Y, Jia Y, et al. Common and specific abnormalities in cortical thickness in patients with major depressive and bipolar disorders. EBioMedicine. 2017;16:162-71.
Figures