1991
Analysis of resting-state networks alterations of first-episode obsessive–compulsive disorder patients by independent component analysis1The First Affiliated Hospital of Zhengzhou University, Zhengzhou, China
Synopsis
So far, there is no consensus on the cause of obsessive-compulsive disorder(OCD). We used a data-driven method, independent component analysis (ICA), to study the change of whole brain resting-state functional connectivity of first-episode and treatment-naïve patients with OCD. Three abnormal resting-state networks, posterior default-mode network, right frontoparietal network and lateral visual network, have been found in patients. In addition, patients showed increased functional connection in bilateral cuneus, right inferior parietal lobule and right middle occipital lobule compared with controls. It’s considered that changes of abnormal resting-state networks might reveal the possible neural mechanism of OCD.
Introduction
Obsessive-compulsive disorder (OCD) is a psychological disorder with an estimated lifetime prevalence of 1% to 3%,1 characterized by uncontrollable obsessive thoughts, compulsive behavior and compulsions to counteract these thoughts and behavior clinically. 2 As known that, OCD is among the leading causes of functional disability worldwide, but the neurobiology and aetiological origins of it is not clear. Recently, a specific network of cortical-striatal-thalamic-cortical (CSTC) circuits has been suggested in the pathophysiology of OCD. 3 However, many of the previous resting-state functional magnetic resonance imaging (rs-fMRI) studies in OCD depended on prior knowledge. Whether there are any other OCD-related functional changes occurring besides the CSTC circuits remains unknown. This study intend to investigate the whole brain rs-fMRI connectivity alternation of first-episode and treatment-naïve OCD patients by independent component analysis (ICA) to explore the pathophysiology of OCD.Methods
A total of 47 subjects were recruited including 23 drug-naive OCD patients and 24 healthy controls with matched age, gender, handedness and education level in this study. OCD patients were diagnosed through Structured Clinical Interview for DSM-IV Axis I Disorders-Non-patient Edition (SCID-I) by an experienced psychiatric chief physician.MRI datasets were acquired on a 3T GE Discovery 750 System (GE Healthcare, Milwaukee, MI, USA) scanner equipped with an 8-channel parallel head coil. Functional MRI data were obtained via a gradient echo-planar imaging sequence (repetition time = 2000 ms; echo time = 30 ms; slices = 32; thickness = 4 mm; resolution matrix =64 × 64; flip angle = 90º; field of view = 220 × 220 mm2; slice gap = 0.5 mm., 180 time points, 5760 images in acquisition , 6 minutes total time). Subjects were instructed to stay alert and relaxed with eyes closed and no body motion during imaging sessions.
Standard image data preparation and pre-processing were performed with MRIcroN software (http://www.mricro.com) and DPARSFA software based on MATLAB 2012b (http://www.mathworks.com). Group ICA was using rs-fMRI image with the Group ICA of fMRI Toolbox (GIFT) (http://icatb.sourceforge.net). Statistical analysis was carried out with SPM8 software (http://www.fil.ion.ucl.ac.uk/spm). One-sample T-test(family wise error correction, p<0.05) was performed to make masks of networks component, and two-sample T-test(alphasim correction, p<0.05) was performed to seek the significant difference of functional networks between OCD patients and controls.
Results
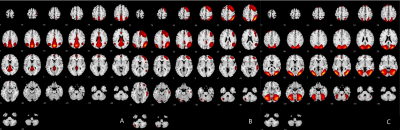
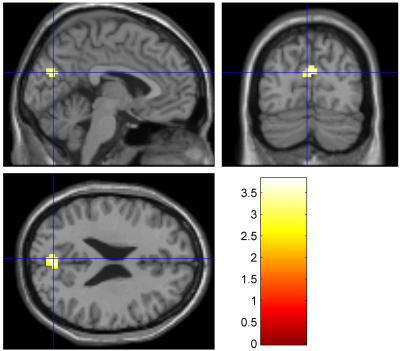
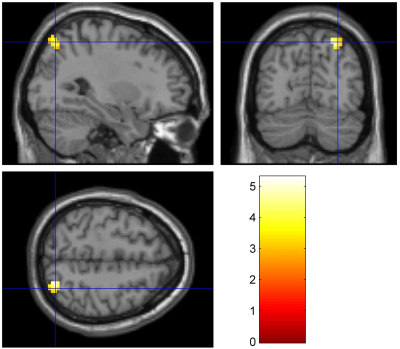
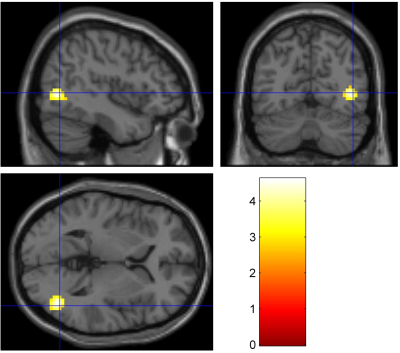
10 masks of resting-state networks were found in both groups. The resting-state networks, posterior default-mode network (pDMN), right frontoparietal network (RFP) and lateral visual network(lVN), appeared significantly difference compared with control group, were shown in Figure 1.The current results showed that the functional connectivity (FC) of pDMN network in OCD patients was higher than that in healthy controls in bilateral cuneus(T=3.822,P=0.005)(Figure 2). The FC of RFP network in the right inferior parietal lobule was higher than that in healthy controls(T=5.291,P=0.005)(Figure 3). Besides, the FC of lVN in the right middle occipital lobule was higher than that in healthy controls(T=4.614,P=0.005)(Figure 4). The alternation of FC had no correlation with Y-BOCS scores.
Discussion
The results of whole brain resting states functional networks in OCD patients without drug and psychosocial interventions showed more objective and reliable information for psychological mechanism of OCD. Noise was removed effectively, and altered brain connectivity between the first-episode and treatment-naïve OCD patients and health controls was found without any priori assumptions and model driven by using ICA. This study revealed that there were three abnormal resting state networks, pDMN, RFP and lVN, which mainly represented increased functional connectivity in OCD patients.Conclusion
Our current provided further evidence of FC abnormalities that are not only present in the classical CSTC circuit but also besides the CSTC circuit, which may represent the complex interaction of abnormally functional organization of networks in OCD. It is believe that this noninvasive method might be useful for exploring the pathophysiology of OCD.Acknowledgements
No acknowledgement found.References
1. Ruscio AM, et al. (2010). The epidemiology of obsessive—compulsive disorder in the National Comorbidity Survey Replicatio. Mol Psychiatry. 15:53-63.
2. Burdick KE, et al. (2008). Neurocognitive profile analysis in obsessive compulsive disorder. J Int Neuropsychol Soc. 14:640–645.
3. Menzies L, et al. (2008). Integrating evidence from neuroimaging and neuropsychological studies of obsessive-compulsive disorder: the orbitofronto-striatal model revisited. Neurosci Biobehav Rev. 32:525-549.
Figures