1913
Combined Co-occurrence of Local Anisotropic Gradient Orientations (CoLlAGe) and Pyradiomics features to predict the prognosis of gliomas.1Department of Medical Imaging, Jinling Hospital, Nanjing University School of Medicine, Nanjing, China, 2Jiangsu Key Laboratory of Big Data Analysis Technique and CICAEET, Nanjing University of Information Science and Technology, Nanjing, China
Synopsis
We tried to establish a model based on features extracted from Pyradiomic framework and Co-occurrence of Local Anisotropic Gradient Orientations (CoLlAGe) in MRI to predict the prognosis of gliomas. Fifty-five pathologically confirmed glioma patients were retrospectively collected. All patients underwent 3DTI enhancement, standardized treatment and follow-up for overall survival. 1781 Pyradiomic features and 260 CoLlAGe features were collected. Three Cox proportional hazards models were fitted with Pyradiomics features, CoLlAGe features and Pyradiomics+CoLlAGe features. The C-index in these models were 0.835, 0.820 and 0.844, respectively. The model with Pyradiomics+CoLlAGe features demonstrated improved survival predictive performance than the single model.
Methods: Fifty-five pathologically confirmed glioma patients (WHO 2016 CNS tumor classification guidelines3: II–IV grades) were retrospectively collected from December 2015 to December 2017. All patients underwent 3DTI enhancement, standardized treatment and follow-up for their overall survival (OS). Manually segmented VOIs of tumor based on 3DTI enhanced images yielded 1781 Pyradiomic features and 260 CoLlAGe features per patient. We used Least Absolute Shrinkage and Selection Operator (LASSO) method4-6 to select features that were most significant to build predictive models for prognosis of patients. Three Cox proportional hazards models were fitted with Pyradiomics features, CoLlAGe features, Pyradiomics+CoLlAGe features, with 10-fold outer-loop-cross-validation, which was repeated 100 times. In addition, each model also includes clinical features such as gender, age and pathological grade. Harrell's C-index was used to quantitatively evaluate the prediction ability of three models, so as to obtain the optimum model for predicting prognosis. Figure 1 shows the whole workflow of this study.
Result: LASSO selection (Figure 2) yielded eight relevant features in Pyradiomics and CoLlAGe features models, and the top four features were included in the Cox proportional hazards models respectively (Table 1). The C-index in the Cox proportional hazards model based on Pyradiomics features, CoLlAGe features and Pyradiomics+CoLlAGe features were 0.835, 0.820 and 0.844, respectively. Nomogram for predicting the prognosis of gliomas in the model of Pyradiomics+CoLlAGe features was shown in Figure 3.
Conclusion: CoLlAGe features extracted from 3DT1 enhancement can be used for predicting the prognosis of gliomas. The model with Pyradiomics+CoLlAGe features demonstrated improved survival predictive performance than the single model, thus suggesting Pyradiomics and CoLlAGe features as MR imaging biomarker in prognosis glioma.
Acknowledgements
The scientific guarantor of this publication is Zhiqiang Zhang. This research was approved by the local medical ethics committee, and written informed consent was obtained from each participant. This study was supported by National Natural Science Foundation of China (Grant nos. 81530054, 81871345, U1809205, 61771249, 81871352), Natural Science Foundation of Jiangsu Province of China (Grant nos. BE2016751, BK20181411), Chinese post-doctor foundation (2016M603064), Post-doctor foundation Jiangsu province (1501169B).References
1. Prasanna P, Tiwari P, Madabhushi A. Co-occurrence of Local Anisotropic Gradient Orientations (CoLlAGe): A new radiomics descriptor. Sci Rep. 2016 Nov 22;6:37241.
2. Prasanna P, Tiwari P, Madabhushi A. Co-occurrence of local anisotropic gradient orientations (CoLIAGe): distinguishing tumor confounders and molecular subtypes on MRI. Med Image Comput Comput Assist Interv. 2014;17(Pt 3):73-80.
3. Louis DN, Perry A, Reifenberger G, et al. The 2016 World Health Organization Classification of Tumors of the Central Nervous System: a summary. Acta Neuropathol. 2016 Jun;131(6):803-20.
4. Zhang B, Tian J, Dong D, et al. Radiomics Features of Multiparametric MRI as Novel Prognostic Factors in Advanced Nasopharyngeal Carcinoma. Clin Cancer Res. 2017;23(15):4259-4269.
5. Hepp T, Schmid M, Gefeller O, et al. Approaches to regularized regression - a comparison between gradient boosting and the Lasso. Methods Inf Med, 2016;55:422–30.
6. Sasaki T, Kinoshita M, Fujita K, et al.Radiomics and MGMT promoter methylation for prognostication of newly diagnosed glioblastoma. Sci Rep. 2019 Oct 8;9(1):14435.
Figures
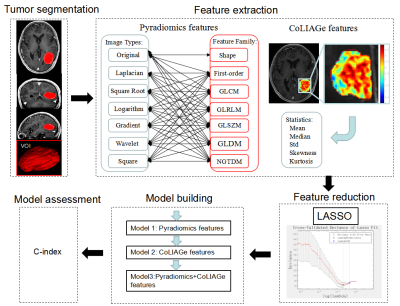
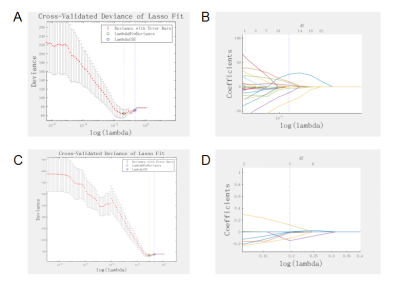
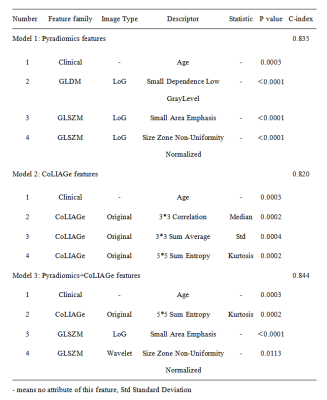
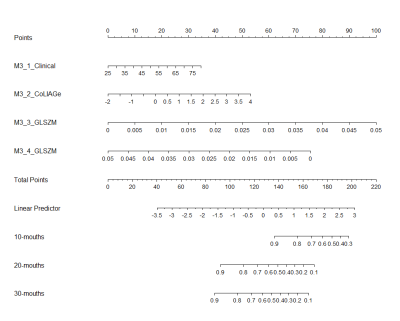
Figure 3. Nomograms for predicting the prognosis of gliomas in the model of Pyradiomics+CoLlAGe features.