1816
Correlation analysis between brain iron deposition and physiological parameters in hypertensive patients1XI’AN DAXING HOSPITAL, ShaanXi, Xi’an, China, 2Siemens Healthcare Ltd, ShaanXi, Xi’an, China, 3Siemens Healthcare Ltd., Beijing, China
Synopsis
Hypertension is becoming a common health problem worldwide with increasing life expectancy and increasing prevalence of risk factors. Hypertension was positively associated with body mass index. Previous studies have detected that increased iron accumulation mainly in deep gray matter nucleus and CSF in hypertensive patients. There has no study about the correlates of physiological parameters and magnetic susceptibility of brain in hypertension. The present study used Pearson's correlation test to compare the relationship between the magnetic susceptibility of brain tissue and BMI, maximum systolic blood pressure and maximum diastolic blood pressure in hypertensive patients.
Introduction
Hypertension is not only a well-known risk factor for cardiovascular disease but also a public health challenge worldwide1. A multivariate logistic regression analysis indicated that high body mass index (BMI) was a risk factor for hypertension. Arterial blood pressure (BP) is largely a surrogate for cerebral perfusion pressure. Extreme arterial hypertension or hypotension is clearly deleterious to multiple organ systems. Multiple studies had investigated the relationship between various BP parameters and clinical outcomes. Previous studies had detected that increased iron accumulation mainly happened in deep gray matter nucleus and CSF in hypertensive patients. Quantitative susceptibility mapping (QSM) can accurately reflect the spatial distribution of the tissue’s magnetic susceptibility, providing an indirect way of quantifying iron content in the brain. Few studies discussed the relationship between QSM of brain tissue and physiological parameters such as BMI, maximum systolic blood pressure and maximum diastolic blood pressure in hypertensive patients. Therefore, the present study aimed to estimate the correlation of physiological parameters and hypertension.Methods
24 patients (12 males, 12 females; mean age = 65.3 ± 10.8 years)with hypertension were recruited in this study. All participants underwent MR scanning on a 1.5T MR scanner (MAGNETOM Aera, Siemens Healthcare, Erlangen, Germany) using a 16-channel head coil. A multi-echo gradient echo (ME-GRE) sequence was applied for QSM acquisition with the following parameters: repetition time (TR) = 51 ms, TE1/ΔTE/TE8 = 8.22 ms/5 ms/43.22 ms, bipolar readout, slice thickness = 2 mm, flip angle = 20°, FOV = 230 mm × 210 mm, matrix size = 224 × 180, bandwidth = 200 Hz/Px, and slices = 56. The magnitude and phase images from ME-GRE acquisition were post-processed to generate susceptibility maps using the MEDI toolbox on Matlab (R2016b, Mathworks, Natick, MA, USA). The regions of interest at the bilateral dental nucleus (DN), dorsal thalamus (TH), putamen (PU), globus pallidus (GP), caudate (CA) and cerebrospinal fluid (CSF) within the lateral ventricle were manually drawn to acquire magnetic susceptibility on the susceptibility maps. Statistical analysis was performed using SPSS software (version 19.0, IBM Corp., Armonk, NY, USA). The measurement data were expressed as mean ± standard deviation (SD). The Kolmogorov-Smirnov test was used to analyze the normality of the data. Correlation between the magnetic susceptibility of brain tissue and BMI, maximum systolic blood pressure and maximum diastolic blood pressure in hypertensive patients (HP) were examined by Pearson's correlation test. A value of p < 0.05 was considered statistically significant.Results
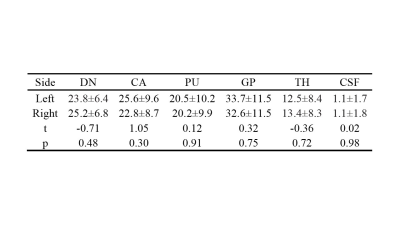
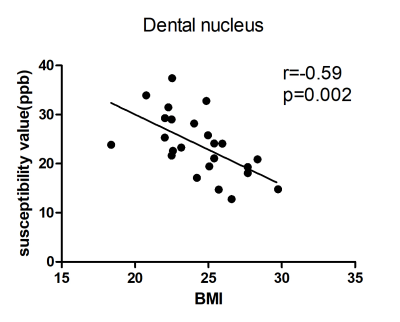
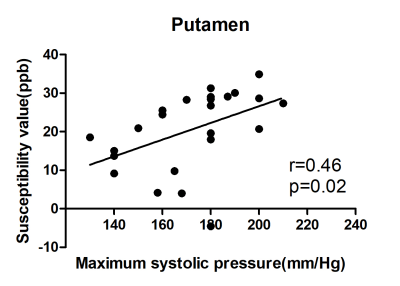
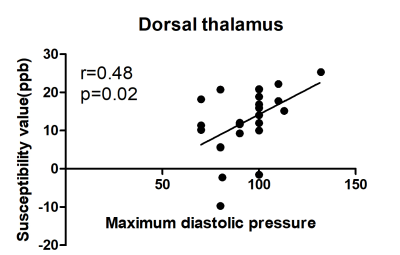
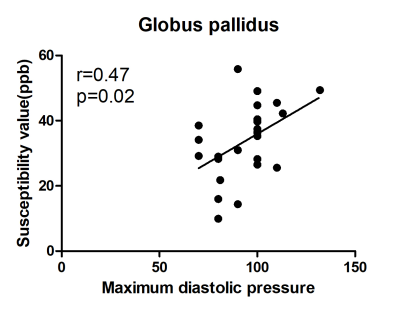
We found that magnetic susceptibility of HP was no statistically significant difference in bilateral DN, TH, PU, GP, CA and CSF in HP patients(p>0.05,Table 1). BMI was significant negatively correlated with susceptibility values in DN (r=-0.59, p=0.002, Fig.1). Maximum systolic blood pressure was significant positively correlated with susceptibility values in PU (r=0.46, p=0.02, Fig.2). Maximum diastolic blood pressure was significant positively correlated with susceptibility values in dorsal thalamus (TH) (r=0.48, p=0.02, Fig.3), globus pallidus (GP) (r=0.47, p=0.02, Fig.4).Discussion
In the present study, we used QSM to analyze the differences of brain iron concentration in hypertensive patients, and estimated the correlates of physiological parameters and hypertension. Our data showed that BMI was significant negatively correlated with susceptibility values in DN. Previous studies found that the prevalence of hypertension increased with increasing body mass index (BMI)2. Our study also discovered that maximum systolic blood pressure was significant positively correlated with susceptibility values in PU. Maximum diastolic blood pressure was significant positively correlated with susceptibility values in dorsal thalamus (TH) and globus pallidus (GP). Considered that high blood pressure is a modifiable risk factor amenable to lifestyle interventions and relatively inexpensive medications, evidence-based blood pressure management is an important strategy for the prevention of stroke. Cohort studies performed in Asian, populations have shown significant associations between systolic blood pressure and mortality and between systolic blood pressure and risk of cardiovascular diseases3. Control of blood pressure in hypertension is recognized as a key measure in the management of cardiovascular risk and is a cornerstone of preventive strategies4.Conclusion
The quantitative assessment of QSM was demonstrated to be effective for measuring iron content in deep gray matter nucleus to explore the underlying pathologic changes of hypertension. There was significantly correlation between QSM value in specific brain issues and physiological parameters. QSM can indirectly reflect the changes of iron content in the brain, which has a good clinical significance for the evaluation and prognosis of hypertension.Acknowledgements
We thank Shaoyu Wang, Xiang Feng of Siemens Healthcare, Ltd., Xi’an, China, for technical support.References
1.Iadecola C, Yaffe K, Biller J, et al. Impact of Hypertension on Cognitive Function: A Scientific Statement From the American Heart Association. Hypertension 2016; 68(6): e67-e94.
2.Hu L, Xiao H, You C, Li J, Cheng X. Prevalence and Risk Factors of Prehypertension and Hypertension in Southern China. Plos One 2017; 12(1): e0170238.
3.Lawes CMM, Rodgers A, Bennett DA, et al. Blood pressure and cardiovascular disease in the Asia Pacific region. Journal of Hypertension 2003; 21(4): 707-716.
4.Volpe M, Gallo G, Tocci G. Is early and fast blood pressure control important in hypertension management? International Journal of Cardiology 2017; 254: 328.
Figures