Rafael OHalloran1, Laura Sacolick1, Hadrien Dyvorne1, Carole Lazarus1, Samantha By1, Brian Welch1, Bradley A Cahn2, Jill T Shah2, Mercy H Mazurek2, Matthew M Yuen2, Gordon Sze2, W. Taylor Kimberly3, Matthew S Rosen4,5, and Kevin N Sheth2
1Hyperfine Research, Inc., Guilford, CT, United States, 2Yale New Haven Hospital, New Haven, CT, United States, 3Division of Neurocritical Care, Department of Neurology, Massachusetts General Hospital, Boston, MA, United States, 4Athinoula A. Martinos Center for Biomedical Imaging, Department of Radiology, Massachusetts General Hospital and Harvard Medical School, Charlestown, MA, United States, 5Department of Physics, Harvard University, Cambridge, MA, United States
Synopsis
Initial evidence of the feasibility of clinical stroke imaging using a portable 64mT MRI system is presented. Twelve patients with a diagnosis of ischemic stroke diagnosis admitted to a neuroscience intensive care unit were imaged with a portable, point-of-care, MRI system.
Introduction
Despite the higher sensitivity of MRI to diagnose stroke, CT remains the standard of care due to lack of access to MRI. A low-cost, portable, low-field system can increase access to MRI, potentially delivering timely diagnosis of stroke to more patients in settings where MRI is not immediately available. Here we evaluate preliminary brain imaging results from stroke patients acquired with a portable MRI scanner, and present initial evidence of the feasibility of clinical stroke imaging in a neuroscience intensive care unit (Neuro-ICU).Methods
Imaging: A portable 64mT MRI scanner (Hyperfine Research Inc., Guilford, USA) was deployed to the Neuro-ICU at Yale New Haven Hospital. Twelve patients with acute stroke as confirmed by computed tomography or conventional MRI were recruited (M/F=9/3, age=57+/-15) and provided consent under a protocol approved by an institutional review board. Patients underwent an imaging protocol that included DWI (TE/TR=24ms/34ms, 3mmx3mmx5mm resolution, b=840 s/mm2, scan time = 8 min), FLAIR (TE/TR/TI=7ms/4000ms/1400ms, 1.5mmx1.5mmx5mm resolution, scan time = 7 min), and FSE (TE/TR=7ms/2200ms, 1.5mmx1.5mmx5mm resolution, scan time = 7 min), using a 1Tx/8Rx coil. Scanning was performed at the bedside; this is possible because the scanner uses a standard 15A power outlet and doesn’t require a shielded room. Data Analysis: Four patients were excluded from the study due to improper positioning in the system. Images of the remaining 8 subjects were evaluated for the presence or absence of a visible lesion.Results
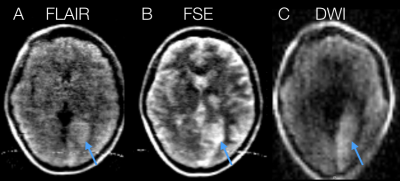
A series of images from subject 1 (left occipital lobe acute evolving infarct) are presented in Figure 1. The lesion is conspicuous and hyperintense on FLAIR, FSE, and DWI (Fig. 1a-c arrows). A small artifact (due to radio-frequency interference) is visible in the lower part of the FSE (Fig. 1a) and FLAIR (Fig. 1b) images. This is due to a standard ECG monitoring system attached to the patient and the lack of a full RF screen around the device. Lesions appeared hyperintense on all contrasts where they were visible. Lesions were visible on FLAIR in 4 of 8 cases, FSE in 7 of 8 cases and in DWI in 7 of 8 cases. The FSE and DWI images that did not show lesions were heavily motion corrupted. All lesions were larger than 7mm along the largest in-plane axis.Discussion and conclusions
Initial imaging results from a 64mT portable MRI scanner show that bedside MRI of stroke may be feasible in lesions larger than 7mm. Patient positioning and motion was an early challenge (resulting in the four discarded cases) that was largely remedied by operator experience and the use of foam padding. An additional limitation of the system is the lower spatial resolution (1.5 mm in-plane for FSE/FLAIR and 3mm in-plane for DWI) due to inherently lower SNR at 64mT. Ongoing work is focused on addressing these issues using motion correction techniques and advanced reconstruction methods. The high rate of lesion conspicuity in these stroke cases is promising evidence that MRI for stroke might one day come to the bedside. Future investigations in larger samples will provide important information regarding the utility of this modality for bedside stroke detection.Acknowledgements
This work was supported by research funding from Hyperfine Research, Inc and an American Heart Association Collaborative Science Award (17CSA33550004).References
No reference found.