1700
Magnetic Resonance Fingerprinting for Preoperative Differentiation of Soft and Hard Meningiomas1Department of Medical Imaging, Henan Provincial People’s Hospital & Zhengzhou University People’s Hospital;Henan Key Laboratory of Neurological Imaging, Zhengzhou, China, 2MR Collaboration, Siemens Healthcare Ltd., Beijing, China, 3MR Pre-development, Siemens Healthcare, Erlangen, Germany, 4Cooperative Innovation Center of Internet Healthcare & School of Software and Applied Technology, Zhengzhou University, Zhengzhou, China
Synopsis
Tumor consistency is an important factor in determining the resectability and surgical outcome of meningiomas. This study investigated the use of magnetic resonance fingerprinting (MRF) to distinguish between meningiomas characterized as soft or hard based on intraoperative patient records. Mann-Whitney U tests were used to compare longitudinal relaxation time (T1) and transverse relaxation time (T2) values derived from MRF. Soft meningiomas had significantly higher T1 and T2 values than hard meningiomas. Both T1 and T2 showed good diagnostic performance, suggesting that MRF may provide valuable information for preoperative differentiation of meningioma consistency and help guide the treatment plan.
Introduction
The best treatment for meningioma is surgical resection. Generally, soft tumors can be easily removed during surgery, while hard tumors often require lengthy and tedious resection[1]. Therefore, if the consistency of a tumor can be assessed preoperatively, surgery may be planned more effectively, and the value of adjuvant therapy may be evaluated[2]. Magnetic resonance fingerprinting (MRF) enables the direct derivation of tissue characteristics such as proton density and the longitudinal (T1) and transverse (T2) relaxation constants. This study aimed to evaluate the utility of MRF to distinguish between soft and hard meningiomas.Methods
Seventeen patients with pathologically confirmed meningiomas (11 female; mean age, 55.2±10.9 years; age range, 31-72 years) were enrolled in the study. All patients underwent magnetic resonance imaging (MRI) before surgery on a 3T MAGNETOM Skyra scanner (Siemens Healthcare, Erlangen, Germany) equipped with a 20-channel head coil. The MR protocol included the following sequences: conventional MRI (2D T1-weighted, 2D T2-weighted) and a prototype spiral fast imaging with steady-state precession (FISP) MRF (field-of-view (FOV) = 256 x 256 mm2; matrix = 256 x 256; slice thickness = 5 mm; flip angle variable = 0° – 74°; a random repetition time (TR) between 12.1 ms and 15.0 ms; 3000 measurements; 41s/slice; 18 slices). The quantitative T1 and T2 maps were generated by matching the measured MRF signal time course to the dictionary. Tumors were characterized as soft (n=7) or hard (n=10) based on surgical records. Two radiologists blinded to the clinical information analyzed the data independently. Regions of interest (ROIs) were manually drawn on the tumors. Mann-Whitney U tests were used to evaluate differences in the T1 and T2 values between the two groups. P < 0.05 was considered statistically significant. Receiver operating characteristic (ROC) curves were generated and the areas under the curve (AUCs) were calculated to evaluate the efficacy of T1 and T2 values in differentiating soft and hard meningioma.Results
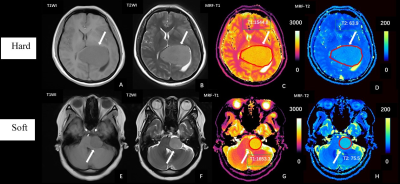
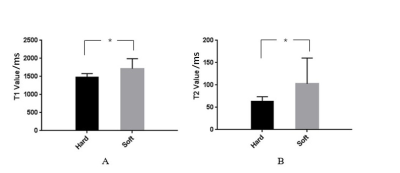
Data from two representative patients with different meningioma consistencies are provided in Figure 1. As shown in Figure 2, the soft meningioma had significantly higher T1 and T2 values than the hard meningioma. The T1 was 1718 ± 273 ms for the soft meningioma versus 1487 ± 91 ms for the hard meningioma (mean ± standard deviation; P=0.008). The T2 was 103 ± 57 ms for the soft meningioma versus 63 ± 10 ms for the hard meningioma (mean ± standard deviation; P=0.022). As shown in Figure 3 and Table 1, the AUCs for T1 and T2 were 0.886 and 0.836, respectively. The T1 value, which had a sensitivity and specificity of 71.4% and 100%, respectively, demonstrated greater diagnostic efficacy than the T2 value.Discussion
Tumor consistency is an important factor in determining the resectability of meningiomas and hence, surgical outcomes[1]. Therefore, the consistency of a meningioma may greatly influence the neurosurgeon's treatment plan. Conventional MRI studies have obtained controversial results, and some investigators have concluded that MRI cannot be used to definitively determine tumor consistency[2]. We used MRF to demonstrate that soft meningiomas have significantly higher T1 and T2 values than hard meningiomas. Additionally, both T1 and T2 values provided good diagnostic performance, with T1 demonstrating slightly better diagnostic efficacy.Conclusion
The results of this study suggest that the quantitative T1 and T2 values derived from MRF have the potential to distinguish soft from hard meningiomas before surgery, which may be valuable in establishing a treatment plan for meningioma.Acknowledgements
This research was supported by the National Key R&D Program of China (2017YFE0103600), National Natural Science Foundation of China (81720108021, 81601466), and Zhongyuan Thousand Talents Plan Project-- Basic Research Leader Talent (ZYQR201810117).References
[1]. Phuttharak W, Boonrod A, Thammaroj J, et al. Preoperative MRI evaluation of meningioma consistency: A focus on detailed architectures[J]. Clinical neurology and neurosurgery, 2018, 169: 178-184.
[2]. Alyamany M, Alshardan M M, Jamea A A, et al. Meningioma consistency: Correlation between magnetic resonance imaging characteristics, operative findings, and histopathological features[J]. Asian journal of neurosurgery, 2018, 13(2): 324.
Figures