1675
Investigation of chemotherapy-induced brain volume and shape change in breast cancer women1Department of Medical Imaging and Radiological Sciences, Chang Gung University, Taoyuan, Taiwan, 2School of Medicine, Chang Gung University, Taoyuan, Taiwan, 3Department of Psychiatry, Chang Gung Memorial Hospital, Chiayi, Taiwan, 4Department of Diagnostic Radiology, Chang Gung Memorial Hospital, Chiayi, Taiwan, 5Medical Imaging Research Center, Institute for Radiological Research, Chang Gung University and Chang Gung Memorial Hospital at Linkou, Taoyuan, Taiwan
Synopsis
Adjuvant chemotherapy has been associated with cognitive impairment among a subgroup of breast cancer patients. A limited number of studies have observed the relationship between adjuvant chemotherapy, post-traumatic stress disorder (PTSD) and structural brain changes. Therefore, we employed voxel-based morphometry (VBM) and vertex-wise shape analyses to find the differences in brain volume and shape among pre- and post-chemotherapy breast cancer patients and healthy subjects. Our results showed gray and white matter volume alterations in frontal and temporal brain regions among each group. We also observed the change of shape in the limbic system.
Introduction
Breast cancer (BC) is the most prevalent cancer for women around the world. The majority of patients with breast cancer have cognitive impairment during and after chemotherapy. Furthermore, patients after chemotherapy who were found cognitive deficits suggest a change in brain structure that affects brain function. An increasing number of studies have used functional neuroimaging methods, such as functional magnetic resonance imaging (fMRI) to investigate regional brain activity and brain functional connectivity 1,2. Moreover, diffusion tensor imaging (DTI), a neuroimaging method, has been used to study cerebral white matter integrity 3,4. However, little is known about the brain volume and shape changes between breast cancer patients before and after receiving adjuvant chemotherapy. Moreover, post-traumatic stress disorder (PTSD), one aftereffect of cancer, also affects cognition ability in breast cancer patients. Therefore, we tried to find the differences in brain volume and shape among pre- and post-chemotherapy breast cancer survivors and healthy subjects using voxel-based morphometry (VBM) and vertex-wise shape analyses.Methods
This study included 45 women with breast cancer before chemotherapy, 58 breast cancer survivors exposed to chemotherapy and 60 healthy control women. All of them performed MRI examination using 3T imaging system (Verio, Siemens, Germany), and the MPRAGE sequence was used to obtain the T1WI. In Voxel-Based Morphometry (VBM), all raw data were processed by Statistical Parametric Mapping 8 (SPM8, Wellcome Department of Cognitive Neurology, London, UK) with Voxel-Based Morphometry 8 (VBM8, University of Jena, Department of Psychiatry, Jena, Germany) toolbox. Each raw data was first normalized to the East Asian Brain template from International Consortium for Brain Mapping, and then segmented into the gray and white matter. Moreover, ages, education years and whole brain volume were used as covariates to avoid the original difference of each brain. The two-sample t-test was used to find the changes of the gray and white matter among each group.In the vertex-wise shape analysis, we used FMRIB Software Library (FSL, Oxford, UK) to segment the brain into 15 specific subcortical structures based on T1-weighted images using shape and appearance models. Then vertex-wise analysis was performed to show the location of differences among each group.Results
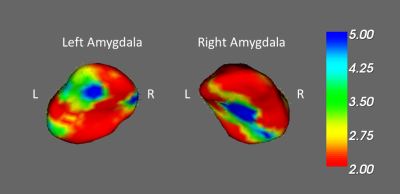
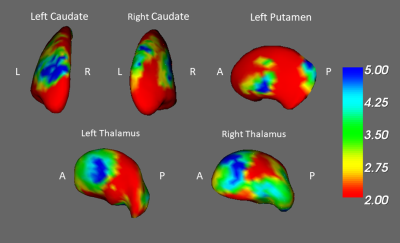
In the result of VBM, we found a smaller volume of the cerebellum, smaller white matter volume of postcentral gyrus and right amygdala in the pre-chemotherapy BC patients compared with healthy controls (Fig. 1). Compared to the post-chemotherapy group, we observed that the volume of the left frontal lobe, superior temporal gyrus, and the posterior cingulate gyrus are larger in the pre-chemotherapy BC patients (Fig. 2). We also discovered the reduced volume of the cerebellum, superior temporal gyrus and cingulate gyrus in the BC patients after chemotherapy compared with healthy controls (Fig. 3). Above the outcomes were all statistically significant (corrected p < 0.03).In the shape analysis, the bilateral amygdala was significantly different in the BC patients before chemotherapy compared with the healthy controls (Fig. 4). Besides, the significant difference was found in the bilateral caudate, bilateral thalamus and left putamen between pre- and post-chemotherapy BC patients (Fig. 5).
Discussion
Our study found the significant structural difference in the frontal lobe, the temporal gyrus and posterior cingulate gyrus between BC patients before and after chemotherapy. The cognitive functions of frontal lobes include motor function, problem solving, memory, judgment, and social behavior. Previous functional studies also indicated frontal lobes are sensitive to chemotherapy 5,6. The more brain volume loss indicated the poor cognitive performance 7. The current study also discovered the temporal region is associated with attention function, and adjuvant chemotherapy affects the brain network and reduces attention abilities in patients 8. It was consistent with our results that the superior temporal gyrus was smaller in post-chemotherapy BC patients. Moreover, cingulate gyrus is a component of the limbic system. Previous studies found it involved with memory integration and observed lower functional connectivity in the patients exposed to chemotherapy 9. It can explain why patients following prolonged chemotherapy would have cognitive deficits. We also discovered the shape abnormality in the limbic system between pre- and post-chemotherapy groups. The limbic system involved in emotional response, memory, learning, and decision-making. The alterations may result from chemotherapy and explain the cause of cognitive impairment. Compared with the healthy controls, a reduced volume of the cerebellum and amygdala were discovered in the pre-chemotherapy groups. Previous neuroimaging studies showed PTSD was related to the cerebellum and amygdala 10,11. It supported brain alteration may be related to PTSD.Conclusion
Adjuvant chemotherapy may affect brain structure and result in cognitive problems. We found a significant difference in the brain volume and the shape of the limbic system in the BC patients before and after chemotherapy among each group. Besides, the brain structural and shape alterations between pre-chemotherapy BC patients and healthy controls may due to PTSD. The result provided evidence that breast cancer and chemotherapy are associated with brain structural alterations and enhanced the importance of the side-effects of chemotherapy and cancer-related trauma.Acknowledgements
This study was supported by the research grants MOST108-2813-C-182-041-B, MOST107-2221-E-182-054-MY3, MOST106-2221-E-182-079, and MOST104-2314-B-040-001 from the Ministry of Science and Technology, Taipei, Taiwan. This study was also supported by grants BMRPD1H0102 and BMRPD1G1322 from Chang Gung University, Taoyuan, Taiwan and CORPG6G0102 and CORPG6G0122 from Chang Gung Memorial Hospital, Chiayi, Taiwan.References
1. Miao H, Li J, Hu S, et al. Long-term cognitive impairment of breast cancer patients after chemotherapy: A functional MRI study. European Journal of Radiology 2016;85:1053-7.
2. Mo C, Lin H, Fu F, et al. Chemotherapy-induced changes of cerebral activity in resting-state functional magnetic resonance imaging and cerebral white matter in diffusion tensor imaging. Oncotarget 2017;8:81273-84.
3. Deprez S, Amant F, Yigit R, et al. Chemotherapy-induced structural changes in cerebral white matter and its correlation with impaired cognitive functioning in breast cancer patients. Human Brain Mapping 2011;32:480-93.
4. Deprez S, Amant F, Smeets A, et al. Longitudinal assessment of chemotherapy-induced structural changes in cerebral white matter and its correlation with impaired cognitive functioning. J Clin Oncol 2012;30:274-81.
5. Dumas JA, Makarewicz J, Schaubhut GJ, et al. Chemotherapy altered brain functional connectivity in women with breast cancer: a pilot study. Brain imaging and behavior 2013;7:524-32.
6. de Ruiter MB, Reneman L, Boogerd W, et al. Late effects of high-dose adjuvant chemotherapy on white and gray matter in breast cancer survivors: converging results from multimodal magnetic resonance imaging. Human brain mapping 2012;33:2971-83.
7. Lepage C, Smith AM, Moreau J, et al. A prospective study of grey matter and cognitive function alterations in chemotherapy-treated breast cancer patients. SpringerPlus 2014;3:444.
8. Chen X, He X, Tao L, et al. The attention network changes in breast cancer patients receiving neoadjuvant chemotherapy: Evidence from an arterial spin labeling perfusion study. Scientific reports 2017;7:42684.
9. Dumas JA, Makarewicz J, Schaubhut GJ, et al. Chemotherapy altered brain functional connectivity in women with breast cancer: a pilot study. Brain Imaging Behav 2013;7:524-32.
10. Rabellino D, Densmore M, Theberge J, McKinnon MC, Lanius RA. The cerebellum after trauma: Resting-state functional connectivity of the cerebellum in posttraumatic stress disorder and its dissociative subtype. Hum Brain Mapp 2018;39:3354-74.
11. Nutt DJ, Malizia AL. Structural and functional brain changes in posttraumatic stress disorder. J Clin Psychiatry 2004;65 Suppl 1:11-7.
Figures