1672
Longitudinal study on changes of regional cerebral blood flow in patients maintaining hemodialysis1Tianjin First Central Hospital;Tianjin Medical Imaging Institute, Tianjin,, Tianjin, China, 2Qinghai University Affiliated Hospital, QingHai, China
Synopsis
This was the first study focused on longitudinal CBF changes of ESRD patients with regular hemodialysis. This study used noninvasive pulsed arterial spin labeling technique to provide evidence for clinical evaluation of the changes in cerebral hemodynamics in hemodialysis patients.
Introduction
To study the changes of regional cerebral blood flow (CBF) in end stage renal disease (ESRD) patients who received maintenance hemodialysis. Pulsed arterial spin labeling (pASL) was used to compare the longitudinal changes of regional CBF of ESRD patients, and changes of regional CBF of ESRD patients with health controls.Materials and Method
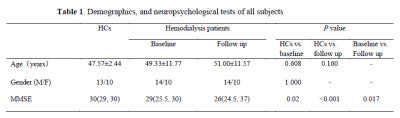
This study included 24 ESRD patients who received regular hemodialysis as patients group and 23 age- gender-, and education level matched health volunteers as health controls (HCs) group. The first examination of ESRD patients was recorded as baseline group, and the follow-up examination was recorded as follow-up group. Siemens Trio Tim 3.0T magnetic resonance scanner was used to collect the images of all the subjects. The patients group underwent MR examination one day before hemodialysis and their clinical laboratory examinations were collected within one week of MR examination. First, conventional MR sequences, including T2WI and T2WI and FLAIR were applied to exclude the congenital cerebral abnormalities. Then, high resolution 3D sagittal T1-weighted images and pASL were obtained. HCs group did not collect clinical laboratory examinations. MMSE tests which was widely used to define cognitive function of ESRD patients [1-3] were evaluated within 30 minutes before MR examination. Statistical parametric mapping 12 (SPM12) based on MATLAB software was used to process ASL and CBF imaging data and make statistical analysis. The differences of CBF values in different brain regions between patients group and HCs group, baseline group and follow-up group were compared. We used SPSS17.0 statistical software to analyze the difference of neuropsychologic scores, age, gender between all three groups, the difference of clinical laboratory examinations between baseline group and follow-up group were also analyzed. The correlation analysis between regional CBF and neuropsychologic scores were analyzed by Spearman correlation analysis. The correlation between regional CBF and clinical laboratory examinations were observed by stepwise multiple linear regression analysis.Result
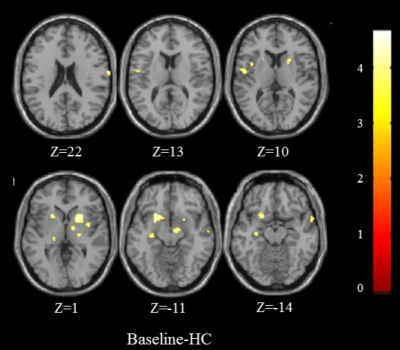
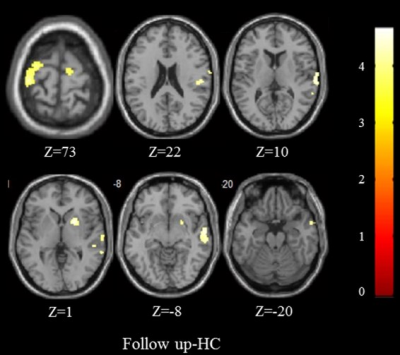
Compared with HCs group, baseline group showed increased CBF in bilateral putamen, bilateral thalamus, bilateral insular lobe, right globus pallidus, right postcentral gyrus, right superior temporal pole, right superior temporal gyrus, left hippocampus and left Rolandic operculum (age and gender as covariates, P=0.001) (Figure 1). Compared with HCs group , follow-up group showed increased CBF in right temporal pole, right superior temporal gyrus, right middle temporal gyrus, right putamen, right globus pallidus, right posterior central gyrus, right Rolandic operculum, left superior frontal gyrus, left precentral gyrus and right supplementary motor area (age and sex as covariates, P=0.001) (Figure 2). Compared with baseline group, the CBF of right postcentral gyrus obviously increased in follow-up group (age as a covariant, P=0.001) (Figure 3). The MMSE scores of patients were significantly lower than those in HCs group (Mann-Whitney U test, both P<0.05) (Figure 4), and those in follow-up group were significantly lower than baseline group (Wilcoxon signed-rank test, P=0.017) (Table 1). There was no significant correlation between MMSE score and regional CBF among the three groups(P>0.05). In baseline group, hemoglobin was an independent risk factor for CBF changes in right temporal pole (β=-0.496, P=0.026), left hippocampus (β=-0.502, P=0.024), left putamen (β=-0.535, P=0.015); hematocrit was an independent risk factor for CBF changes in right thalamus (β=-0.536, P=0.015), left thalamus (β=-0.569, P=0.009); urea was an independent risk factor for CBF changes in right superior temporal gyrus (β=-0.542, P=0.014);creatinine was an independent risk factor for CBF changes in right globus pallidus (β=-0.703, P=0.001), right insular lobe (β=-0.482, P=0.031) and left insular lobe (β=-0.537, P=0.015). In follow-up group, parathyroid hormone was an independent risk factor for CBF changes in right temporal pole (β=-0.449, P=0.047); hemoglobin was an independent risk factor for CBF changes in right middle temporal gyrus(β=-0.605, P=0.005), right postcentral gyrus(β=-0.533, P=0.015), right superior frontal gyrus (β=-0.589, P=0.006), right superior temporal gyrus (β=-0.546, P=0.013), right putamen (β=-0.536, P=0.015), left precentral gyrus (β=-0.602, P=0.005).Conclusion
The difference of CBF between ESRD patients and HCs was studied by pASL technique. It was found that regional CBF increased and cognitive function decreased in ESRD patients. In compared with baseline group, it showed that increasing CBF in right postcentral gyrus within follow-up group. Creatinine, urea, hemoglobin and hematocrit may be independent risk factors for CBF changes in baseline group. Parathyroid hormone and hemoglobin may be independent risk factors for CBF changes in follow-up group. In this study, noninvasive pASL technique was used to monitor the longitudinal CBF changes in ESRD patients, and to provide evidence for clinical evaluation of the changes in cerebral hemodynamics in hemodialysis patients.Acknowledgements
No acknowledgement found.References
1. Chai C, et al. Increased number and distribution of cerebral microbleeds is a risk factor for cognitive dysfunction in hemodialysis patients: a longitudinal study. Medicine 2016; 95.
2. Chao C, et al. Increased brain iron deposition is a risk factor for brain atrophy in patients with haemodialysis: a combined study of quantitative susceptibility mapping and whole brain volume analysis. Metab Brain Dis 2015; 30:1009-1016.
3. Chai C, et al. Reduced regional cerebral venous oxygen saturation is a risk factor for the cognitive impairment in hemodialysis patients: a quantitative susceptibility mapping study[J]. Brain Imaging Behav 2018: 1-11.
Figures