1671
Brain atrophy was a risk factor for neurocognitive impairment in hemodialysis patients: a longitudinal voxel-based morphological study1Radiology, Tianjin First Central Hospital;Tianjin Medical Imaging Institute, Tianjin,, Tianjin, China, 2Qinghai University Affiliated Hospital, QingHai, China, 3Tianjin First Central Hospital;Tianjin Medical Imaging Institute, Tianjin,, Tianjin, China
Synopsis
This study aimed to demonstrate the longitudinal changes of brain volume in hemodialysis, and the relationship between brain volume and cognitive function. Thirty-three hemodialysis patients and thirty healthy controls (HCs) were recruited to this study. All patients underwent MR examinations to evaluate baseline and follow-up brain volume. Compared to the HCs, patients showed decreased gray matter (GM) volume and white matter (WM) volume. Compared to baseline patients, follow-up patients showed decreased GM volume and WM volume. The decreased left caudate volume was positively correlated with reduced neuropsychological scores in patients. Brain atrophy occurred in hemodialysis patients, leading to neurocognitive impairment.
Introduction
To explore longitudinal changes of brain volume in hemodialysis patients, the risk factors for brain volume changes, and the relationship between brain volume changes and results of neuropsychological test.Materials and Method
A total of 41 hemodialysis patients were recruited from the Hemodialysis Center of Tianjin First Central Hospital from November 2015 to July 2019. The inclusion criteria were : 1) age: all subjects were 18 years or older; 2) handedness: all subjects were right-handed; 3) MRI results: subjects had no contraindications to MR examination; 4) study completion: all patients completed the baseline and follow-up examinations; all available MRI data were complete, including high resolution 3D sagittal T1-weighted imaging, transversal T2-weighted imaging (T2WI), and fluid attenuated inversion recovery (FLAIR) imaging; 5) history of ESRD: the dialysis duration of patients was more than 3 months without history of peritoneal dialysis or kidney transplantation. The exclusion criteria included: 1) inability to complete the MR examinations; 2) comorbidities: the subjects had other diseases affecting brain volumes, such as infarction, hematoma, and trauma; the subjects had neurodegenerative diseases, such as Alzheimer’s disease, and Parkinson’s disease; 3) abnormal brain structures: congenital abnormalities of brain structures were found in routine MRI examinations; 4) image quality: the image quality was too poor to perform VBM analysis. Based on the inclusion and exclusion criteria, 33 patients were enrolled (Figure 1). Each patient underwent the first examination at baseline. Then patients underwent second examinations at follow-up. All patients received regular hemodialysis therapy for four hours each time, three times a week. Thirty age-, gender-, and education-matched HCs were recruited from local communities in Tianjin.To investigate the clinical risk factors for the brain volume changes in hemodialysis patients, blood biochemical examinations were performed. The blood biochemical indices included hematocrit, serum urea, serum creatinine, serum phosphorus, alkaline phosphatase, β2-microglobulin, and parathyroid hormone. No blood biochemical tests were performed on HCs. In order to assess neurocognitive function of all subjects, Mini-mental State Examination (MMSE) tests [1-3] were performed with MR scanning.
All MRI data were acquired on a 3 T MR imager (MAGNETOM Trio a Tim System, Siemens Healthcare, Erlangen, Germany). All subjects were required to keep their head immobile during the MR examination. First, conventional MR sequences, including T2WI and T2WI fluid attenuated inversion recovery (FLAIR) were applied to exclude the congenital cerebral abnormalities, occupying-space diseases, and demyelinating diseases. Then, high resolution 3D sagittal T1-weighted images were obtained by magnetization-prepared rapid gradient-echo (MP-RAGE) sequence.
Results
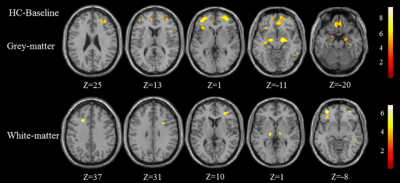
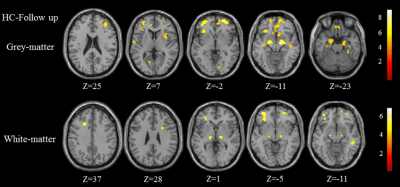
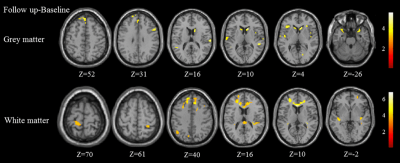
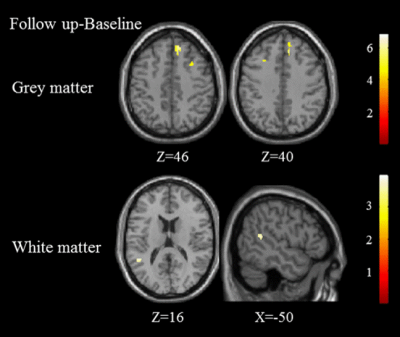
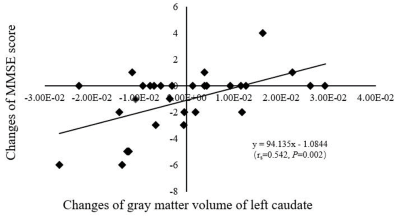
Compared to the HCs, patients at baseline and follow-up showed decreased gray matter (GM) volume and decreased white matter (WM) volume (FWE corrected with age, gender and total intracranial volume [TIV] as covariates, P<0.05) (Figure 1&2). Compared to baseline patients, follow-up patients showed diffusely decreased GM volume and decreased WM volume (with age and TIV as covariates, uncorrected, P=0.001) (Figure 3. In our study, we also found increased GM volumes in the bilateral frontal lobes and WM volumes of the left temporal lobe in patients at follow-up compared with patients at baseline (with age and TIV as covariates, uncorrected, P=0.001) (Figure 4). Creatinine, urea, hematocrit, parathyroid hormone and alkaline phosphatase were independent risk factors for decreased brain volume in patients (all P<0.05). The decreased left caudate volume was positively correlated with reduced neuropsychological scores in patients (rs=0.542, P=0.002) (Figure 5).Conclusion
Our study was the first study that focused on the longitudinal changes of brain volume in hemodialysis patients. We found decreased GM and WM volume in hemodialysis patients at baseline and follow-up compared with HCs. We also found GM and WM atrophy in patients at follow-up compared to patients at baseline. In our study, it was also found that increased GM volumes in the bilateral frontal lobes in patients at follow-up compared with patients at baseline, a finding which was consistent with Johansen et al.’s cross-sectional study [4]. We found that MMSE scores of patients at follow-up were significantly lower compared to those of patients at baseline, and the changes in of left caudate nucleus volume between two examinations were significantly positively correlated with the changes in MMSE scores, indicating that brain atrophy resulted in the progressive neurocognitive impairment as the result of hemodialysis therapy. Creatinine, urea, hematocrit, parathyroid hormone and alkaline phosphatase were independent risk factors for decreased brain volume in patients. Brain atrophy occurred in hemodialysis patients, leading to neurocognitive impairment.Acknowledgements
No acknowledgement found.References
1. Chai C, et al. Increased number and distribution of cerebral microbleeds is a risk factor for cognitive dysfunction in hemodialysis patients: a longitudinal study. Medicine 2016; 95.
2. Chao C, et al. Increased brain iron deposition is a risk factor for brain atrophy in patients with haemodialysis: a combined study of quantitative susceptibility mapping and whole brain volume analysis. Metab Brain Dis 2015; 30:1009-1016.
3. Chai C, et al. Reduced regional cerebral venous oxygen saturation is a risk factor for the cognitive impairment in hemodialysis patients: a quantitative susceptibility mapping study[J]. Brain Imaging Behav 2018: 1-11.
4. Johansen N, Kjaergaard KD, Peters CD, Pedersen M, Jespersen B, Jensen JD. Brain swelling during dialysis: A randomized trial comparing low-flux hemodialysis with pre-dilution hemodiafiltration. Clin Nephrol 2017; 87 (2017):221.
Figures