1659
Cerebral perfusion territory changes after artery recanalization in unilateral MCA stenosis disease: a territory arterial spin labeling study
Xinyu Wang1, Xinyi Wang2, and Weiqiang Dou3
1Medical imaging, Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan,Shandong, China, 2Medical imaging, The First Affiliated Hospital of Shandong First Medical University, Jinan,Shandong, China, 3MR Research China, GE Healthcare, Beijing, China
1Medical imaging, Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan,Shandong, China, 2Medical imaging, The First Affiliated Hospital of Shandong First Medical University, Jinan,Shandong, China, 3MR Research China, GE Healthcare, Beijing, China
Synopsis
In this study, the main purpose was to explore the clinical value of territory arterial spin labeling (T-ASL) in assessing perfusion changes after unilateral middle cerebral artery (MCA)recanalization. We included 15 patients diagnosed by Digital Substraction Angiography(DSA) with unilateral MCA stenosis, T-ASL examination was performed before and after surgery. Patients showed significantly different reperfusion areas between pre- and post-operations, and some had hyperperfusion displacement in the major cerebral arterial blood supply area. Therefore, T-ASL technique can be used as a valuable method to evaluate the effect of vascular recanalization accurately.
Introduction
Unilateral middle cerebral artery(MCA)stenosis is very common and has many causes. Usually, balloon dilation or stent implantation is used in interventional surgery to restore blood flow to different degrees. Digital Substraction Angiography(DSA)is often used as gold standard to evaluate the effect of vascular recanalization. However, DSA is an invasive technique with radiation and also requires contrast agent. T-ASL, as a relative novel non-invasive MRI method, can be used to measure different perfusion areas by labeling specific arteries1-3. This technique has been often used for evaluation after Moyamoya disease (MMD) vascular reconstruction4. It remains however unknown if this technique is also feasible to evaluate the recanalization of vascular stenosis. Therefore, the main purpose of this work was to use T-ASL technique to explore the changes of cerebral blood perfusion in patients with unilateral MCA stenosis before and after. We hypothesized that the T-ASL technique could provide accurate information about the perfusion territory changes of the major cerebral arteries and would be comparable to DSA in postoperative evaluation.Methods
SubjectsFrom January 2019 to August 2019,15 patients (6 males vs 9 females; mean age: 49±6.541 years old) with unilateral MCA stenosis were included in this study. All patients were diagnosed by DSA before surgery,and the length of vascular stenosis was measured at the same time . All patients have undergone balloon dilation or stent implantation.
MRI experiment
All patients received two MRI examinations before and after the operation. All the scans were performed on the 3.0T MRI scanner (GE Discovery 75, USA) equipped with a 32-channel head coil. A 3D pseudo-continuous arterial spin labeling based T-ASL sequence was applied to respectively measure the blood perfusion in right and left internal carotid arteries. The corresponding scan parameters included: field of view =220 mm×220 mm; slice thickness=4.0 mm; repetition time =4548 ms; labelling duration= 1,450 ms; post-labelling delay =1525 ms; arms =4; and number of excitations=2. The acquisition time for the T-ASL scheme was approximately 3minutes and 20seconds . The vascular markers selected in TASL measurement were a section of bilateral internal carotid arteries(ICAs)running perpendicular to the axial plane.
Image Analysis
In ADW 4.6 workstation (GE Medical systems), the T-ASL images were post-processed using a vendor-provided tASL post-processing software. The cerebral blood flow (CBF) maps of each labeled vessel (i.e., right and left ICAs) were obtained before and after surgery accordingly. The preoperative and postoperative perfusion areas of the same blood vessels were aligned and compared to assess the perfusion changes. The maximum level of hypoperfusion in the blood supply area was selected at the affected side of the internal carotid artery and the area was measured. Two regions of interest (ROI)s with an area of (150±10) mm²were also chosen. The corresponding CBF values were measured and then averaged for data analysis.The increased perfusion area due to blood flow redistribution after surgery was defined as the reperfusion area (RA). If RA was detected in the ipsilateral hemisphere, the condition was defined as RA positive. Otherwise, RA was considered negative.
Statistical Analysis
In SPSS software, Pearson correlation analysis was used to evaluate the relationship between the length of vascular stenosis and reperfusion area. Paired t test was used to respectively compare the difference between hypoperfusion area and mean CBF value before and after surgery. Significance threshold was set as p <0.05.
Results
Preoperative TASL showed decreased perfusion in cerebral hemisphere of the narrowed arteries relative to the contralateral side in 15 patients. Among them, 12 (80%) TASL patients showed reperfusion area (RA positive), and the rest 3 (20%) patients did not show reperfusion area (RA negative). A typical case is shown in Figure 1.Using Pearson correlation analysis, high correlation coefficient (r=﹣0.896, P<0.01) was obtained between the length of vascular stenosis and the reperfusion area(Figure 2). The hypoperfusion area at the affected side of the cerebral hemispheric blood supply region after surgery was significantly reduced compared with that before surgery, and the corresponding CBF was also increased than that before the operation(Table 1), with statistically significant difference (both p<0.05).Discussion and conclusion
In this study, vessel specific perfusion imaging of patients before and after surgery revealed an increase in perfusion area due to the redistribution of blood flow, and a return of hyperperfusion areas because of collateral circulation or compensatory blood supply to normal blood supply areas provided by the middle cerebral artery. However, there are still several patients without reperfusion area. This may be caused by short postoperative recovery time or the poor effect of surgical recanalization.In conclusion, TASL has demonstrated the clinical value in evaluating the effect of vascular recanalization.Acknowledgements
References
- Gao, X. Y. et al. A perfusion territory shift attributable solely to the secondary collaterals in moyamoya patients: a potential risk factor for preoperative hemorrhagic stroke revealed by t-ASL and 3D-TOF-MRA. J Neurosurg, 1-9, doi:10.3171/2019.5.JNS19803 (2019).
- Lu, Y. et al. Evaluation of the applicability of territorial arterial spin labeling in meningiomas for presurgical assessments compared with 3-dimensional time-of-flight magnetic resonance angiography. Eur Radiol 27, 4072-4081, doi:10.1007/s00330-017-4760-9 (2017).
- Lin, T. et al. ASL perfusion features and type of circle of Willis as imaging markers for cerebral hyperperfusion after carotid revascularization: a preliminary study. Eur Radiol 29, 2651-2658, doi:10.1007/s00330-018-5816-1 (2019).
- Yuan, J. et al. Cerebral Perfusion Territory Changes After Direct Revascularization Surgery in Moyamoya Disease: A Territory Arterial Spin Labeling Study. World Neurosurg 122, e1128-e1136, doi:10.1016/j.wneu.2018.11.002 (2019).
Figures
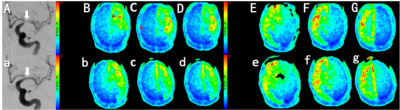
Figure 1:A 57-year-old patient with severe M1 segment stenosis of the left MCA underwent angioplasty, which was a typical RA positive case. (A) preoperative DSA .(B, C, D) preoperative T-ASL:obvious hypoperfusion region in the left cerebral hemisphere(E-G)Preoperative T-ASL: right ICA blood supply distribution. (a) Postoperative DSA.(b,c,d)Postoperative T-ASL : enlarged perfusion area in the left cerebral hemisphere (RA positive), with displacement of the hyperperfusion area. (e-g)postoperative T-ASL: Compared with the previous no significant change.
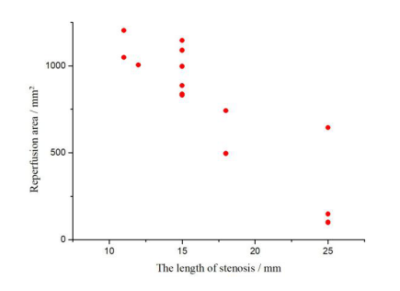
Figure 2 The correlation between the length of vascular stenosis and reperfusion area
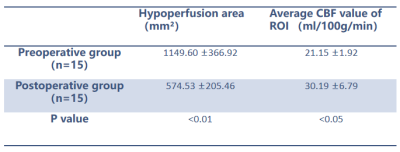
Table 1 The hypoperfusion area in the responsible arterial blood supply area and the average CBF value of ROI were compared between the preoperative group and the postoperative group