1656
Prediction of severe stenosis at the unilateral proximal internal carotid artery by intracranial MR angiography1Radiology, Kyoto Prefectural University of Medicine, Kyoto, Japan, 2Radiology, Kyoto Yamashiro General Medical Center, Kizugawa, Japan
Synopsis
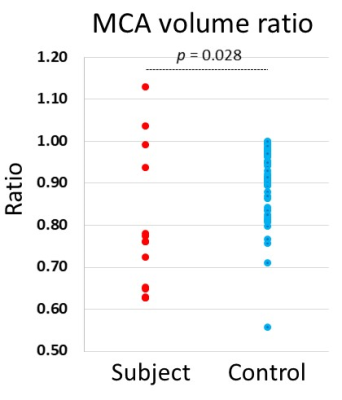
The proximal internal carotid artery (pICA) stenosis is an important cause of ischemic cerebrovascular disease. We evaluated the predicting power to identify unilateral pICA stenosis based on the intracranial 3D time of flight MR angiography (MRA) with multi-slab acquisition used in daily clinical practice by a quantitative assessment of the asymmetry in the middle cerebral artery (MCA). The result revealed that the MCA volume ratio of subjects were significantly lower than controls and the accuracy, sensitivity and specificity to identify subjects were 0.71, 0.71 and 0.88. The quantitative evaluation on intracranial MRA may provide additional information to unilateral pICA stenosis.
INTRODUCTION
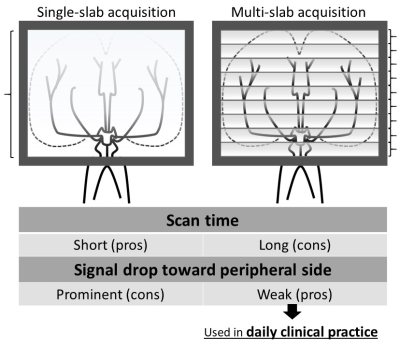
The proximal internal carotid artery (pICA) stenosis is an important cause and risk factor of ischemic cerebrovascular disease (1,2). So it can be a meaningful information to detect pathological condition by conventional intracranial MRA. A previous study concluded that intracranial ICA size asymmetry of 3D time of flight (TOF) MR angiography (MRA) with the single-slab acquisition is an indirect sign of severe cervical ICA stenosis (3). However, it is not common to use the single-slab acquisition in daily clinical practice (Fig. 1). The purpose of this study was to evaluate the predicting power to identify unilateral pICA stenosis based on intracranial 3D TOF MRA with the multi-slab acquisition by a quantitative assessment of the asymmetry on the middle cerebral artery (MCA) area.METHODS
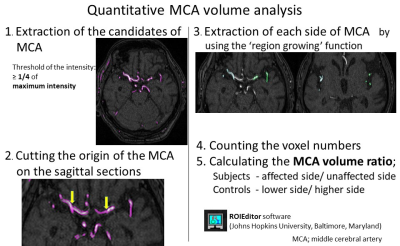
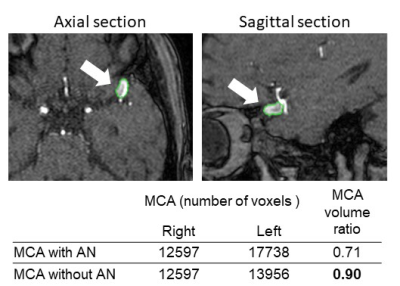
Data acquisition: Fourteen subjects (11 men and 3 women), ranging in age from 58 to 83 (mean ± SD 74.2 ± 7.69) were recruited. The subjects had more than 70 % of unilateral pICA stenosis according to the North American Symptomatic Carotid Endarterectomy Trial (NASCET) criteria on the digital subtraction angiography performed from February 2011 to July 2016. The control group were 34 patients (22 men and 12 women), ranging in age from 49 to 91 (mean ± SD 72.5 ± 8.71) who did not have significant stenoses at both sides of pICA on contrast-enhanced cervical MRA. We also excluded the patients who had severe stenoses in the intracranial arteries. All MRA were obtained on a 1.5-T whole body MR scanner (Gyroscan, Intera, Phillips Healthcare). Three Dimension TOF intracranial MRA acquisitions used a phased array head coil with axial slabs centered on the circle of Willis (TR/TE: 17/6.9 ms; acquisition bandwidth: 114 Hz; flip angle: 116°; field of view: 230×230 mm; matrix: 512×512, acquisition time: 3 min 40 s; slab number 24, axial sections of 0.53 mm thickness). Quantitative analysis (Fig. 2): First, we extracted voxels which had more than one-fourth signal intensity of the maximum intensity among whole slices as candidates of the MCA. Second, we cut off the origin of each side of MCA on the sagittal sections respectively. Third, we extracted only both sides of the MCA itself by using “region growing function”. Fourth, we counted the voxel numbers of each side of the MCA separately. Then, we calculated the MCA volume ratio, which means affected side-to-unaffected side ratio for subjects and lower volume side-to-higher volume side ratio for controls. T-tests were performed for a significant p value < 0.05. The threshold was set to 0.8 of the MCA volume ratio to distinguish subjects from controls.RESULTS
The MCA volume ratio of subjects was significantly lower than that of controls (p = 0.028, Fig. 3). The accuracy, sensitivity and specificity to identify the subjects were 0.71, 0.71 and 0.88, when the threshold was set to 0.8 of the MCA volume ratio.DISCUSSION
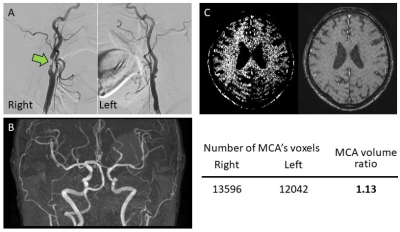
The quantitative volume evaluation showed a good result for the prediction of the ipsilateral pICA stenosis, which were almost equivalent performance to the past study which used MRA with the single slab acquisition (sensitivity and specificity were 0.88 and 0.84 - 0.88) (3). There were some error cases to distinguish subjects from controls. One of the causes of the error cases could be inhomogeneous background signal intensities in the both groups (Fig. 4). Some of error cases had asymmetry in the background signal intensities, which could cause the error. Even though we got wrong results in the normal cases because of inhomogeneity, we could make a correct decision because human can take those effects into consideration during interpretation. The other reason of the error cases was an aneurysm (Fig. 5). The control case with the aneurysm had a large asymmetry in the MCA volume, which led to exceed the threshold we set. After we excluded the aneurysm from the MCA volume, the asymmetry disappeared. We can easily recognize those error cases before our final judgement. In this study, there are several limitations. First, this was a retrospective study. Second, MRA was performed only with the 1.5 T MR scanner. Third, we excluded cases that had bilateral stenoses at the pICA or intracranial artery stenoses. Fourth, there could be compensation flows form the anterior and/or posterior communicating artery. For the future directions, we would like to improve the methods of computational evaluation by using artificial intelligence techniques to extract each side of MCA and interpret intracranial MRA together with this computational volume evaluation and the visual evaluation.CONCLUSION
The quantitative volume evaluation of the asymmetry of the MCA may provide additional information on unilateral pICA stenosis on the intracranial MRA with the multi-slab acquisition.Acknowledgements
No acknowledgement found.References
1. de Weerd M, Greving JP, Hedblad B, Lorenz MW, Mathiesen EB, O'Leary DH, Rosvall M, Sitzer M, Buskens E, Bots ML. Prevalence of asymptomatic carotid artery stenosis in the general population: an individual participant data meta-analysis. Stroke; a journal of cerebral circulation 2010;41(6):1294-1297. 2. Flaherty ML, Kissela B, Khoury JC, Alwell K, Moomaw CJ, Woo D, Khatri P, Ferioli S, Adeoye O, Broderick JP, Kleindorfer D. Carotid artery stenosis as a cause of stroke. Neuroepidemiology 2013;40(1):36-41.
3. Naggara O, Touze E, Seiller N, Gobin-Metteil MP, Mas JL, Meder JF, Oppenheim C. Asymmetry of intracranial internal carotid artery on 3D TOF MR angiography: a sign of unilateral extracranial stenosis. European radiology 2008;18(5):1038-1042.
Figures