1649
MRI features of cerebral small vessel disease in patients with systemic lupus erythematosus1Department of Radiology, The First Affiliated Hospital of Dalian Medical University, Dalian, China, 2Department of Radiology, GE healthcare, Beijing, China
Synopsis
Systemic lupus erythematosus (SLE) is a diffuse connective tissue disease, which can involve the nervous system, and cerebrovascular damage is the most common. Yet, the relationship between SLE and Cerebral small vessel disease (CSVD) are still not clear. The following study evaluated the MRI findings of enlarged perivascular space (EPVS), white matter hyperintense (WMH) and lacunes of CSVD in patients with SLE. The results showed that CVSD in SLE group was more serious than healthy normal control group, and complement C3 and disease duration were the influencing factors on the development of CSVD in SLE patients.
Introduction
Systemic lupus erythematosus is an autoimmune immune-mediated diffuse connective tissue disease that involves multiple systems and organs 1. When the nervous system is involved, SLE can cause cerebrovascular damage, which in turn may increase the risk of stroke 2. CSVD is a clinical syndrome caused by intracranial small blood vessels (≤ 2 mm in diameter). Its imaging features include recent occurring subcortical infarction and white matter hyperintense (WMH), lacune of presumed vascular origin, enlarged perivascular space (EPVS), cerebral microbleeds, and brain atrophy. So far, many studies have focused on investigating SLE cerebrovascular changes associated with large and middle cerebral arteries of the head and neck, while the imaging features of cerebral small vessel disease remain unexplored. In this study, we analyzed the presence of CSVD in the brain of SLE patients and healthy controls, and explored the occurrence of CSVD in SLE patients and its clinical influencing factors.Materials and Methods
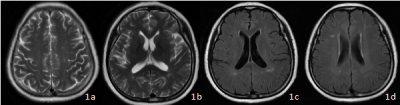
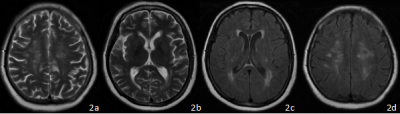
Twenty-nine SLE patients (2 males and 27 females, mean age 43.82±12.99 yrs) and twenty-nine age- and sex-matched healthy subjects (2 males and 27 females, mean age 45.14±9.73 yrs) were enrolled in this retrospective study. All subjects underwent routine MRI scans. EPVS, WMH, and lacunes were rated by two radiologists.( Figure 1,2) Kappa test was used to verify the consistency of the evaluation results of two radiologists. SPSS 24 was used for statistical analyses; Kolmogorov-Smirnov Z test was used to analyze group difference, while the relations between CSVD and clinical & laboratory finding were analyzed using Spearman correlation.Results
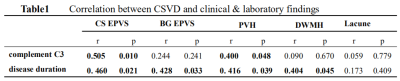
In the centrum semiovale (CS), the EPVS score in the SLE patients was higher compared to the healthy ones (2.52±0.91, 1.34±0.55, P<0.01). The periventricular hyperintense (PVH) and deep white matter hyperintense (DWMH) in the SLE group were more serious than in the healthy subjects (P<0.01). Lacunes occurred more often in the SLE's than in the controls (P<0.05). Moreover, in SLE group, EPVS in the CS and PVH was associated with complement C3 (r=0.505,0. 400,P<0.05); and EPVS and WMH were positively correlated with disease duration (r=0. 460, 0. 428, 0. 416, 0.404, P<0.05). (Table1)Discussion
This study used semi-quantitative enumeration and grading to assess the number of EPVS, lacunes and WMH in the brain of SLE patients and normal controls. The results showed that the EPVS score in the semi-oval center of the brain; the burden of WMH and the incidence of lacunes were all significantly higher in the SLE group compared to the healthy controls, which further confirmed that SLE patients were at higher risk of CSVD compared to healthy controls.The main pathophysiological mechanism of brain damage in patients with SLE is the autoantibody-mediated inflammation 3. Antibodies related to SLE may bind to endothelial cells 4, affect the blood-brain barrier, and allow inflammatory factors to enter the brain, thus increasing EPVS. Extensive active lupus may lead to extensive vascular inflammation and endothelial dysfunction, as well as deep cerebral arteriolar stenosis and occlusion, resulting in white matter changes and visible lacunes on MRI. Previous studies have shown that CSVD burden is increased in SLE patients 5. This study also found that CSVD burden is related to complement C3, thus suggesting that SLE inflammatory activity has an effect on PVH production. The course of SLE is related to the occurrence of EPVS and WMH in the brain, which suggests that the length of the disease duration is one of the influencing factors on the development of cerebral small vessel disease in SLE patients.
Conclusion
Cerebral small vessel disease is a common manifestation of central nervous system lesions in SLE patients that is associated with complement C3 and disease duration.Acknowledgements
No acknowledgement found.References
1. Tsokos GC. Systemic lupus erythematosus[J]. N Engl J Med, 2011,365(22): 2110-2121.
2.Wiseman S J, Ralston S H, Wardlaw J M. Cerebrovascular disease in rheumatic diseases: a systematic review and meta-analysis[J]. Stroke, 2016, 47(4): 943-950.
3.Ramage A E, Fox P T, Brey R L, et al. Neuroimaging evidence of white matter inflammation in newly diagnosed systemic lupus erythematosus[J]. Arthritis & Rheumatism, 2011, 63(10): 3048-3057.
4.Kowal C, DeGiorgio L A, Lee J Y, et al. Human lupus autoantibodies against NMDA receptors mediate cognitive impairment[J]. Proceedings of the National Academy of Sciences, 2006, 103(52): 19854-19859.
5.Wiseman S J, Bastin M E, Jardine C L, et al. Cerebral small vessel disease burden is increased in systemic lupus erythematosus[J]. Stroke, 2016, 47(11): 2722-2728
Figures