1639
Intense Ostium Hemodynamics as the Potential Causes for Delayed Occlusion of Unruptured Sidewall Intracranial Aneurysms by Flow Diverter1Interventional radiology, Beijing Friendship Hospital, Capital Medical University, Beijing, China, 2Neuroradiology and Neuro-interventional radiology, University Hospitals of Geneva, Geneva, Switzerland
Synopsis
Flow diverter (FD) has recently been introduced for cerebral aneurysms, especially for the uncoilable sidewall type in the tortuous internal carotid artery (ICA). However, some of treated aneurysms remain patent in clinical practices, probably because of hemodynamic reason. Four-dimensional phase contrast sequences (4D flow MRI) targeting the aneurysm bulge were prospectively performed. The results showed that intense hemodynamic effect at the aneurysmal neck and large ostium might need a longer time for FD induced occlusion. 4D flow MRI before FD procedures has the potential to depict and quantify ostium hemodynamics that could bring new insights in characterizing their treatment responses.
Purpose
Intracranial aneurysm can lead to a potential devastating outcome. Flow diverter (FD) has recently been introduced for cerebral aneurysms[1], especially for the uncoilable sidewall type in the tortuous internal carotid artery (ICA). However, some of treated aneurysms remain patent in clinical practices[2], probably because of hemodynamic reason.Therefore, this study used 4D phase contrast (PC) MRI, a powerful in vivo analytic tool[3], to explore the aneurysmal hemodynamics and their outcome. The purpose of our study was to perform an in vivo investigation of the relationship between aneurysmal features (hemodynamic and geometric) and their impact on FD treatment responses.
Methods
We conducted a prospective study of 41 consecutive patients diagnosed with unruptured sidewall intracranial aneurysm and accepted for a FD procedure according to our inclusion and exclusion criteria. Three patients were excluded because of MRI acquisition problem or FD subsequent displacement.Four-dimensional phase contrast sequences (4D flow MRI) targeting the aneurysm bulge were prospectively performed for each patient using a 3.0 T scanner (Ingenuity TF, Philips Healthcare, Cleveland, OH) within 72 hours before flow diverter treatment. This sequence triggered with the cardiac frequency included velocity encoding in the three directions. Three dimensional rotational angiograms (3DRA) were acquired before FD stent implantation with an angiographic unit.
The vessel lumen was segmented using an interactive watershed analysis performed on the gradient of the reconstructed 3DRA volume. After raw data post-processing from the 4D PCMRI and 3DRA, velocity field information and the parent vessel flow rate were acquired for further analysis.
FD selection was determined by navigability and implantation issues. No combination of coils was used. FDs were deployed by an experienced neurointerventionist, followed by a cone bean CT to confirm its proper deployment.
Two follow-ups imaging were successively acquired at 6 and 12-month after the FD implantation. According to 6- and 12-month CE-MRI or DSA follow-ups with a simplified two-grade scale[4], FD-treated aneurysms were classified as either “occlusion” or “remnant”. All investigations were blinded to the acquisition parameters from the follow-ups.
Each aneurysmal ostium plane was defined as the location from which the aneurysmal sac bulged outward from its parent vessel. According to velocity field information, hemodynamic parameters at the aneurysmal neck were evaluated on open-source software Paraview (version 5.6.0; Kitware, NY). Geometric parameters were measured on pre-procedural 3DRA images. Hemodynamic and geometric parameters were compared between the two groups and analyzed with the receiver operating characteristic curve.
Results
Patient DemographicsThirty-eight patients (mean age, 53.7 years ± 13.4, [range, 26–81 years]) with 41 target aneurysms underwent subsequent FD procedures and were included in the study. In three patients, two target aneurysms were close to each other and one FD was deployed for both of them to achieve the coverage of two ostiums at the same time. Apart from one middle cerebral artery aneurysm (M1 segment), aneurysms were situated in the ICA from C4 to C7 segments (Bouthillier nomenclature).
Follow-ups
After 6- (173.7 days ± 48.1) and 12-month (367.8 days ± 83.4) follow-ups, 21 aneurysms and 30 aneurysms were occluded, respectively. Finally, 40 aneurysms were screened for comparison at 6 and 12 months.
Hemodynamic Qualitative Comparison
Qualitative analyses at the aneurysmal neck revealed that the cases with an inflow zone on the proximal neck in the remnant group were statistically more frequent than cases with other inflow zones at 6 months (P=0.004), but not statistically at 12 months (P=0.126).
Hemodynamic Quantitative Comparison
For hemodynamic quantitative parameters at the ostium, there were significant differences in maximum inflow velocity, maximum inflow rate, systolic inflow rate ratio, and the systolic inflow area at 6-month. Statistically significant differences for maximum inflow rate, systolic inflow rate ratio, systolic inflow area, and the parent vessel flow rate were observed at 12 months. The most pronounced differences were identified for the systolic inflow rate ratio and systolic inflow area at 6 and at 12 months, respectively.
Geometric Comparison
There were significant differences in aneurysm sac size, perpendicular height, maximum height, ostium maximum diameter, ostium area and size ratio at 6 and 12 months. Among them, ostium maximum diameter showed the most pronounced difference.
ROC Prediction
As predicting parameters with ROC for the occlusion and remnant group, the areas under the curves (AUCs) of systolic inflow rate ratio and ostium maximum diameter reached 0.855 (95% confidential interval [CI]: 0.735–0.974, P<0.001) and 0.843 (95% CI: 0.707–0.980, P<0.001), respectively, at 6 months. AUCs of systolic inflow area and ostium maximum diameter at 12 months were 0.860 (95% CI: 0.730–0.990, P=0.001) and 0.883 (95% CI: 0.759–1.000, P<0.001), respectively. Based on the Youden index for favorable sensitivity and specificity, the optimal predictive cutoff was 0.343 for the systolic inflow rate ratio and 4.9 mm for ostium maximum diameter at 6 months. The optimal predictive cutoff at 12 months was 13.35 mm2 for the systolic inflow area and 4.9 mm for ostium maximum diameter (Fig 1).
Conclusions
Intense hemodynamic effect at the aneurysmal neck and large ostium may need a longer time for FD induced occlusion. 4D flow MRI before FD procedures has the potential to depict and quantify ostium hemodynamics that could bring new insights in characterizing their treatment responses.Acknowledgements
Authors thank Pierre Bouillot (Department of Quantum Matter Physics) and Benedicte M. A. Delattre (Division of Radiology) to provide the MRI sequence optimization. Authors also thank Dr Paolo Machi, Dr Hasan Yilmaz, Dr Gianmarco Bernava, Dr Andrea Rosi and Mr Michel Muster for assistance with angiography. All studies complied with current regulation (including ethics requirements) and laws of the Switzerland.References
[1] Chalouhi N, Tjoumakaris S, Starke RM, et al.Comparison of flow diversion and coiling in large unruptured intracranial saccular aneurysms.Stroke,2013,44:2150-2154.
[2] Madaelil TP, Grossberg JA, Howard BM, et al.Aneurysm Remnants after Flow Diversion: Clinical and Angiographic Outcomes.AJNR Am J Neuroradiol,2019,40:694-698.
[3] Pereira VM, Delattre B, Brina O, et al.4D Flow MRI in Neuroradiology: Techniques and Applications.Top Magn Reson Imaging,2016,25:81-87.
[4] Attali J, Benaissa A, Soize S, et al.Follow-up of intracranial aneurysms treated by flow diverter: comparison of three-dimensional time-of-flight MR angiography (3D-TOF-MRA) and contrast-enhanced MR angiography (CE-MRA) sequences with digital subtraction angiography as the gold standard.J Neurointerv Surg.,2016,8:81-86.
Figures
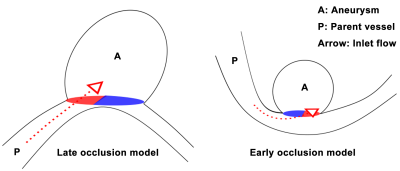
Illustrations of late and early occluded types of aneurysms reported in our results.
Left: a diagram of a late occluded aneurysm shows intense ostium hemodynamics with proximal neck inflow and large sac size, height, ostium in geometries. Right: a diagram of an early occluded aneurysm shows mild ostium hemodynamics with distal neck inflow and less sac size, height, ostium in geometries. Oval red and purple regions at the ostium represent the inward and outward blood flow areas, respectively.