1633
Bright Vessel Appearance on Arterial Spin Labeling MRI: Beyond Localizing Arterial Occlusion1Department of Radiology, Chinese PLA General Hospital, Beijing, China, 2State Key Laboratory of Magnetic Resonance and Atomic and Molecular Physics, National Center for Magnetic Resonance in Wuhan, Wuhan Institute of Physics and Mathematics, Chinese Academy of Sciences‐Wuhan National Laboratory for Optoelectronics, Wuhan, China
Synopsis
Bright vessel appearance on arterial spin labeling (ASL) had been reported to be a useful marker for localizing arterial occlusion in acute ischemic stroke. But ischemia due to cerebral arterial occlusion did not always show bright vessel appearance on ASL. In the present study, we found that the presence of bright vessel appearance may associate with thrombus age and be able to specifically identify acute cerebral arterial occlusion. The findings may help to optimize current stroke protocols and facilitate the diagnosis of fresh thrombus, thus to support the treatment decision making in stroke patients with large vessel occlusion.
INTRODUCTION
Bright vessel appearance (BVA) on arterial spin labeling (ASL) MRI had been reported to be useful for localizing arterial occlusion in acute ischemic stroke.1,2 But ischemia due to cerebral arterial occlusion did not always show bright vessel appearance on ASL. We speculated that bright vessel appearance was correlated with thrombus age. In the present study, we tested the ability of bright vessel appearance to identify acute cerebral arterial occlusion in patients with ischemic stroke. For comparison, we also tested the susceptibility vessel sign (SVS) on susceptibility weighted imaging (SWI) to identify acute cerebral arterial occlusion in these patients as well.METHODS
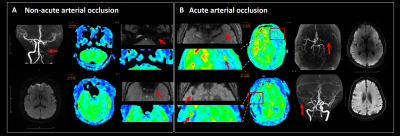
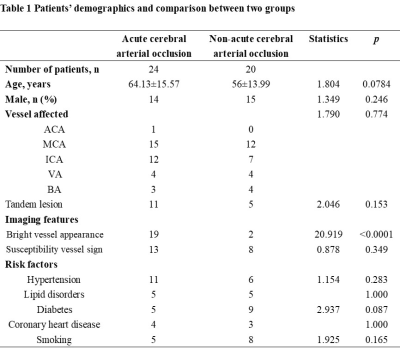
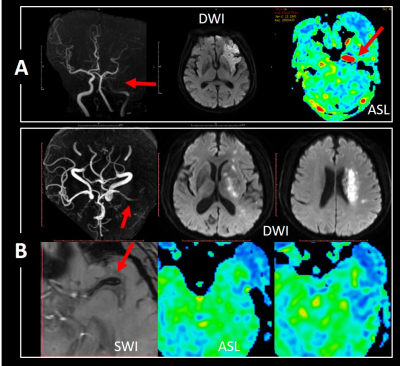
We prospectively recruited patients with symptomatic or asymptomatic cerebral arterial occlusion confirmed by MR angiography (MRA)/computed topography angiography /conventional angiography, who had also undergone MRI including MRA, diffusion-weighted imaging (DWI), pseudo-continuous ASL with post labeling delay of 2.0s and SWI on a 3.0T MR scanner (Discovery 750, GE) from March 2018 to March 2019. Patients were categorized into one of the two groups: patients with acute arterial occlusion, diagnosed as symptom onset to MRI scanning within 24 hours with DWI lesion and vessel occlusion, and patients with non-acute arterial occlusion, confirmed as symptomatic occlusion with symptom onset to MRI scanning exceeding 24 hours or asymptomatic occlusion. BVA on ASL was defined as marked focal or linear hyperintensity within the occlusive vessel route. SVS was defined as the hypointense signal on SWI within the occlusive vessel. Illustrations were shown in Figure 1. The location of a bright spot on ASL was recorded as proximal, distal or both to the thrombus detected by SWI. Clinical variables including age, risk factors and imaging features including vascular lesion location on MRA, the presence of BVA and SVS were compared between the two groups by using student’s t and X2 tests. The receiver operating characteristic curve (ROC) was performed to test the ability to detect acute cerebral artery occlusion of BVA and SVS, and their sensitivity and specificity were also calculated.RESULTS
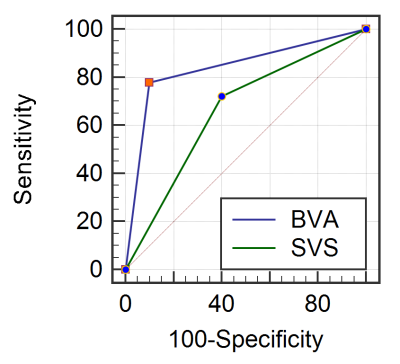
Totally, 44 patients had enrolled in the study. Within them, 21 patients had shown BVA, and 23 patients had shown SVS. Twenty-four patients were categorized as acute cerebral arterial occlusion including 19 BVA positive and 13 SVS positive. Twenty patients were categorized as non-acute cerebral arterial occlusion including 2 BVA positive and 8 SVS positive. The prevalence of BVA between groups was significantly different (79.2% versus 10%, p<0.0001) whereas SVS was not significantly different. Figure 3 shows two cases presenting positive and negative BVA with 7 hours and 7 days from symptom onset. Vascular lesion location on MRA as well as risk factors did not show significant differences between groups. Figure 2 represents Table of patients demographics and comparison between two groups. Area under curve (AUC) was 0.839 (p<0.0001) for BVA to detect acute cerebral arterial occlusion with a sensitivity of 79.2% and specificity of 90%. AUC was 0.661 (p=0.039) for SVS to detect acute cerebral arterial occlusion with a sensitivity of 72.2% and specificity of 60%. ROC analysis was shown in Figure 4. ROC revealed that AUC of BVA was significantly better than that of SVS (p=0.044). In the 12 patients with both BVA positive and SVS positive, BVA located exactly either proximal or distal to the thrombus revealed by SWI.DISCUSSION
To the best of our knowledge, this was the first time to report the association of imaging marker on ASL with thrombus age. Since BVA might result from the labeled water accumulating or diffusing into the thrombus, fresh thrombus could characterize more permeability than the old ones. However, the sensitive to localizing arterial occlusion in acute stroke patients of our study was 79.2% which was lower than 94% as reported in the original paper.1CONCLUSION
Beyond localizing arterial occlusion, the presence of bright vessel appearance may associate with thrombus age. Considering the difficulty in cerebral arterial thrombus age assessment in vivo, the findings may help to optimize current stroke protocols and facilitate the diagnosis of fresh thrombus in stroke patients with large vessel occlusion.Acknowledgements
NoneReferences
1. Yoo R E, Yun T J, Rhim J H, et al. Bright Vessel Appearance on Arterial Spin Labeling MRI for Localizing Arterial Occlusion in Acute Ischemic Stroke. Stroke, 2015, 46(2): 564-567.
2. Majer M, Mejdoubi M, Schertz M, et al. Raw Arterial Spin Labeling Data Can Help Identify Arterial Occlusion in Acute Ischemic Stroke. Stroke, 2015, 46(6): e141-e144.
Figures