1632
Highly Accelerated Compressed Sensing Time-of-Flight MRA for head and neck arterial stenoses: comparison with digital subtraction angiography1Radiology department, The first affiliated hospital of nanjing medical university, Nanjing, China, 2Interventional Radiology department, The first affiliated hospital of nanjing medical university, Nanjing, China, 3MR Collaboration NE Asia, Siemens Healthcare, Shanghai, China, 4Siemens Healthcare GmbH, Erlangen, Germany
Synopsis
As a widely used technique for cerebrovascular disease, the anatomical coverage of TOF-MRA is often limited in order to achieve a compromise between high spatial resolution and acceptable scan time. Compressed sensing (CS) is an effective technique for accelerating 3D acquisitions. In this study, we report the preliminary results of CS TOF-MRA for diagnosing head and neck arterial steno-occlusive disease by taking DSA as the reference standard. CS TOF-MRA provides a relatively large coverage, high resolution, good image quality and comparable diagnostic accuracy to DSA in the assessment of head and neck arterial stenoses within a reasonable acquisition time.
Introduction
Intracranial and extracranial arterial atherosclerotic steno-occlusive disease is an important cause of ischemic stroke1. Digital subtraction angiography (DSA) is the gold standard for accessing vascular stenosis, but it is an invasive and radiation-associated technique2. Time-of-flight magnetic resonance angiography (TOF-MRA) is a widely used and noninvasive technique for diagnosing cerebrovascular disease. However, the spatial coverage is often compromised to achieve a half-millimeter resolution and good signal to-noise ratio, while keeping the scan time clinically acceptable3. Compressed sensing (CS) is a novel technique for undersampling the k-space which allows rapid imaging acquisition4. We aimed to investigate the utility of CS TOF-MRA for diagnosing head and neck arterial steno-occlusive disease by using DSA as the reference standard.Methods
Thirty-seven patients with head and neck arterial stenoses who underwent CS TOF-MRA and DSA were retrospectively enrolled. CS TOF-MRA was performed based on a research sequence and reconstruction prototype on a 3.0 T MR scanner. The scan range was 16 cm, extending from the bifurcation of the common carotid artery to the body of the corpus callosum. The acceleration factor of CS TOF-MRA was set at 10.3. The acquired resolution was 0.6 × 0.6 × 0.6 mm3 and reconstructed to 0.4 × 0.4 × 0.4 mm3. Data were reconstructed using 10 iterations of the Modified Fast Iterative Shrinkage-Thresholding Algorithm. The scan time and reconstruction time was 5 minutes and 2 seconds and 4 minutes and 14 seconds, respectively. The image quality of CS TOF-MRA was independently ranked by two neuroradiologists in 1031 arterial segments. The luminal stenosis grades on CS TOF-MRA and DSA were quantitatively analyzed in 61 arterial segments and were compared using the Wilcoxon signed-rank test. The ability of CS TOF-MRA to predict moderate to severe stenosis or occlusion was analyzed according to receiver-operating-characteristic (ROC) curve analysis.Results
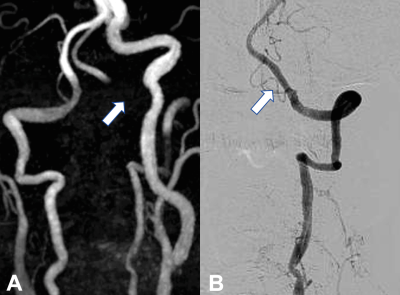
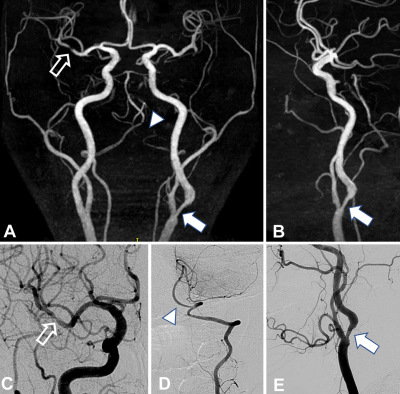
The image quality of most arterial segments (95.2%) on CS TOF-MRA was considered as excellent. Arterial segments with low image quality were mainly the V3 and V4 segments of the vertebral artery (Figure 1). The majority of arterial stenoses (62.3%) were located in proximal internal carotid artery. The luminal stenosis grades of CS TOF-MRA were concordant with that of DSA in 50 of 61 segments (P = 0.366, Figure 2). CS TOF-MRA had a sensitivity of 84.4% and a specificity of 88.5% for predicting moderate to severe stenosis. For detecting occlusion lesions, it had a sensitivity of 100% and a specificity of 94.1%.Discussion
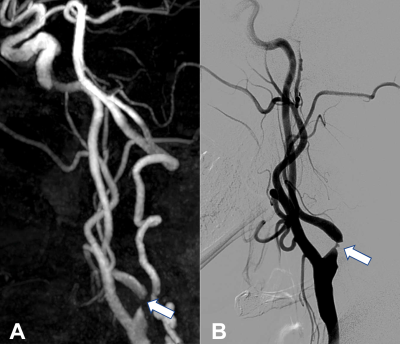
Artifacts of CS TOF-MRA were most commonly observed near the skull base, especially in V3 and V4 segments of vertebral arteries. The possible reasons included susceptibility gradients present in skull base and the slower blood flow through the hypoplasia side of the vertebral artery5-6. Accelerated flow through the stenotic site may lead to dephasing and overestimation of stenosis ratio on CS TOF-MRA5. We considered discontinuity of flow on MIP images as occlusion in the current study, which was the most common cause of overestimating severe stenosis as occlusion (Figure 3). For the underestimation of stenosis using CS TOF-MRA, one possible reason was plaques with hemorrhage might cause a high signal, thus masking signal loss on maximum intensity projection images7. Another reason in our study was unavoidable measurement error when borderline stenosis occurs.Conclusion
CS TOF-MRA provides a relatively large coverage, high resolution and a good image quality of head and neck arteries within a reasonable acquisition time. It may be a reliable tool for diagnosing head and neck arterial steno-occlusive disease.Acknowledgements
No acknowledgement found.References
1. Johnston SC, Mendis S, Mathers CD. Global variation in stroke burden and mortality: estimates from monitoring, surveillance, and modelling. Lancet Neurol. 2009;8(4):345-354.
2. Willinsky RA, Taylor SM, TerBrugge K, et al. Neurologic complications of cerebral angiography: prospective analysis of 2,899 procedures and review of the literature. Radiology. 2003;227(2):522-528.
3. Patel MR, Klufas RA, Kim D, et al. MR angiography of the carotid bifurcation: artifacts and limitations. AJR Am J Roentgenol. 1994;162(6):1431-1437.
4. Lustig M, Donoho D, Pauly JM. Sparse MRI: The application of compressed sensing for rapid MR imaging. Magn Reson Med. 2007;58(6):1182-1195.
5. Anderson CM, Saloner D, Tsuruda JS, et al. Artifacts in maximum-intensity-projection display of MR angiograms. AJR Am J Roentgenol. 1990;154(3):623-629.
6. Nederkoorn PJ, van der Graaf Y, Eikelboom BC, et al. Time-of-flight MR angiography of carotid artery stenosis: does a flow void represent severe stenosis? AJNR Am J Neuroradiol. 2002;23(10):1779-1784.
7. Huston J, Lewis BD, Wiebers DO, et al. Carotid artery: prospective blinded comparison of two-dimensional time-of-flight MR angiography with conventional angiography and duplex US. Radiology. 1993;186(2):339-344.
Figures