1630
Non-enhanced hybrid arterial spin labeling zTE MRA for intracranial arteries: a feasibility study1Northern Jiangsu People’s Hospital, Yangzhou, China, 2GE Healthcare, Beijing, China
Synopsis
In this study, we aimed to investigate the feasibility of a hybrid arterial spin labeling (hASL) zero-echo-time (zTE) magnetic resonance angiography (MRA) for intracranial arteries. Comparing with the conventional zTE MRA (continuous ASL, cASL), the hASL-zTE-MRA showed higher signal homogeneity in the proximal intracranial arteries. Additionally, hASL-zTE-MRA provided more robust performance in depicting cerebrovascular diseases, such as stenosis and arteriovenous malformation (AVM). We therefore demonstrated that the utilization of hASL strategy could potentially improve the image quality of zTE-MRA, and further be applied routinely in the clinic for patients with cerebrovascular diseases.
Introduction
Magnetic resonance angiography (MRA) has been proposed as a promising technique to image intracranial arteries[1]. In particular, zero-echo-time (zTE) MRA, integrated with continuous ASL (cASL) and zTE readout strategy, is insensitive to susceptibility distortion, superb artery selectivity, and silent[2]. One drawback of this technique however, is the appearing of hollowing artifacts or flow void. Hybrid arterial spin labeling (hASL)-zTE MRA has demonstrated its potential in depicting cerebrovascular [3]. Flow void effect was eliminated in hASL-zTE-MRA via continuous inflow of tagged blood during readout. However, whether this sequence is robust and validated in the diagnosis of cerebrovascular diseases remains unclear. Hence, in this study, we aimed to investigate the feasibility of hASL-zTE-MRA quantitatively and qualitatively in the characterization of intracranial arteries of healthy controls, and reported several representative cases of cerebrovascular diseases.Materials and Methods
24 healthy volunteers (11 males & 9 females; 35.92±14.65 years) and 2 patients (a 25-y females and a 47-y males) suspected with cerebrovascular disorders were recruited. All participants received cASL- and hASL- zTE-MRA scanning randomly at the 3.0T GE Discovery 750w MR scanner. In addition, computed tomography angiography (CTA) was also performed as a reference for the cerebrovascular disorders. For fair comparison, the total length of the ASL labeling module was fixed among the two methods (1500 ms) whereas the inversion pulse and inversion time were respectively 1380 ms and 100 ms. Identical zTE acquisition was made for the two cases: FOV/Matrix 180mm/180; spokes per segment 512; flip angle 3o; and bandwidth 31.25 kHz; total scan time 344 seconds. The MRA images were analyzed in the following two steps: 1. Signal to noise ratio (SNR) of the hASL- and cASL- MRAs was estimated respectively. Twenty-nine segments were assessed for each participant, including bilateral internal carotid artery (cervical, petrous, foramen lacerum, cavernous, clinoid process, ophthalmic and traffic segments), bilateral anterior cerebral artery (A1 and A2 segments), bilateral middle cerebral artery (M1 and M2 segments), bilateral posterior cerebral artery (P1 and P2 segments), and basilar artery. 2. The signals homogeneity of each cerebral artery was scored using a 4-point scale (4=excellent, 3=good, 2=poor, 1=not visible) independently by two experienced neuroradiologists. Degree of stenosis was scored on a 3-point scale (1,<50% stenosis; 2, 50%-99% stenosis; and 3, occluded). All statistical analyses were performed using SPSS 19.0 software. The difference of SNR values between each segment of cASL- and hASL- zTE-MRA were evaluated using a paired-samples T test. The ratings of image quality were evaluated using Wilcoxon-signed-rank tests respectively. P<0.05 was considered statistically significant.Results
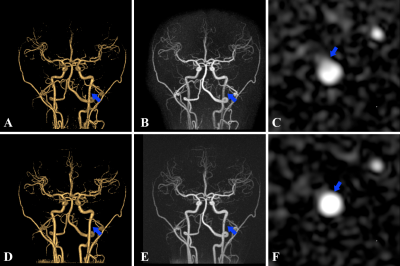
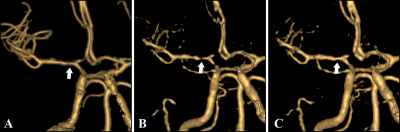
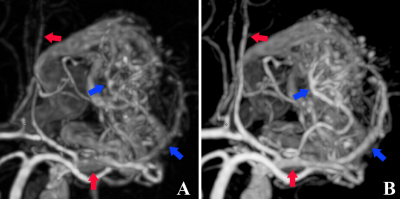
There were no evident vascular diseases within 24 healthy volunteers. In addition, two patients with cerebrovascular disorders were included: 1 stenosis case and 1 arteriovenous malformation (AVM) case. At the segmental level, hASL-zTE-MRA performed well for all intracranial ICA segments and the proximal branches of arterial segments (vertebral artery, M1, A1, P1 segments). In particular, hASL-zTE-MRA showed significantly superior SNR to cASL-zTE-MRA for cervical ICA (10.15±1.50 vs 7.30±1.04; p<0.05) and petrous ICA segments (10.77±1.44 vs 9.12±1.67; p<0.05). The SNR values for hASL-zTE-MRA were also calculated for basilar artery, M2, A2, and P2 arterial segments. Comparable values were revealed relative to those for cASL-zTE-MRA. Mean score of the signals homogeneity for hASL-zTE-MRA (3.56±0.35) was superior scores for cASL-zTE-MRA (3.27±0.44). There was less edge blur effect in depiction of cerebral arteries especially all intracranial ICA segments (Fig.1). For the patient with artery stenosis, hASL-zTE-MRA, compared to cASL-zTE-MRA, showed higher signal homogeneity (3.48±0.29 vs 3.30±0.41; p<0.05). While some lesions might be overestimated on cASL-zTE-MRA, the artery stenosis has been clearly visualized in hASL-zTE-MRA images, of which the quality was equal to that on CTA (Fig.2). 1 AVM patients could be diagnosed, however, hASL-zTE-MRA showed more accurate details than cASL-zTE-MRA (Fig.3).Discussion and conclusion
In this work, we evaluated the feasibility of hASL-zTE-MRA in intracranial arteries by comparing with a conventional cASL-zTE-MRA. While keeping the silent nature of zTE MRA, hASL vessel images didn’t show the hollowing artifact and flow void effect which have been usually appeared in cASL. Moreover, hASL images had higher SNR and less edge blur effect in depiction of proximal branches of intracranial arterial segments. Additionally, hASL showed more robust performance in depicting cerebrovascular diseases, which can improve the accuracy of clinical diagnosis. In conclusion, with these early but promising results, hASL-zTE-MRA has shown a potential to image patients with cerebrovascular diseases in the clinic. To further validate this, studies with a large clinical cohort are requested to be implemented in the near future.Acknowledgements
References
[1]. Bash S, Villablanca JP, Jahan R, et al. Intracranial Vascular Stenosis and Occlusive Disease: Evaluation with CT Angiography, MR Angiography, and Digital Subtraction Angiography. Ajnr Am J Neuroradiol. 2005;26 (5):1012-1021.
[2]. Shang S, Ye J, Dou W, et al. Validation of Zero TE–MRA in the Characterization of Cerebrovascular Diseases: A Feasibility Study[J]. American Journal of Neuroradiology, 2019, 40(9): 1484-1490.
[3]. Qu JX, Wu B, Zhou ZY. Silent Magnetic resonance angiography with hybrid arterial spin labeling techniques. In: Proceedings of the 24th scientific meeting, International Society for Magnetic Resonance in Medicine, Singapore. 2016;p1426
Figures