1624
Apparent PCA territory hypoperfusion on arterial spin labeling MRI is a common artifact in patients with a unilateral fetal PCA.
Abraham Noorbakhsh1 and Divya Bolar1
1Department of Radiology, University of California, San Diego, San Diego, CA, United States
1Department of Radiology, University of California, San Diego, San Diego, CA, United States
Synopsis
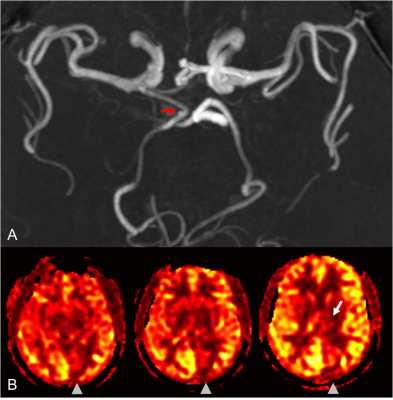
A retrospective review was performed of 50 patients undergoing MRI with pseudo-continuous arterial spin labeling (pCASL) perfusion imaging and confirmed unilateral fetal PCA. The aim is to determine the frequency of visually-apparent unilateral PCA territory hypoperfusion in patients with a contralateral fetal PCA, but without underlying clinical or imaging pathology to suggest true hypoperfusion. Eight of the fifty cases (16%) had visually-apparent hypoperfusion in the PCA territory contralateral to the fetal PCA. Given these findings, we advise caution when interpreting ASL in patients with a fetal PCA/variant circle of Willis anatomy or suggest using longer post-labeling delay times.
INTRODUCTION
Pseudo-continuous arterial spin labeling (pCASL) allows non-contrast assessment of cerebral perfusion and has become a clinically important tool in evaluating neurological disease. However, pCASL is prone to artifacts that can result in erroneous interpretation. Our group periodically encounters visually-apparent unilateral PCA territory hypoperfusion in patients with the normal anatomic variant of a contralateral fetal PCA, but who are without underlying clinical or imaging pathology to suggest true hypoperfusion. The objective of this study is to determine the frequency of this phenomenon in patients scanned with pCASL as part of our institution’s routine brain MRI protocol.METHODS
A search of MRI/MRA reports at our institution from 1/2017 to 3/2019 was performed with inclusion search term of “fetal PCA”, and other terms to exclude patients with significant neuropathology. Of the resulting 70 patients with both MRI and MRA studies, 50 patients were included who had unequivocal unilateral fetal PCAs and diagnostic ASL scans, but without conventional imaging (DWI, FLAIR, or SWI) abnormalities or clinical symptoms referable to the PCA territories. One patient was excluded due to a basilar artery stenosis that resulted in ASL arterial transit artifact. The 50 cases were evaluated by two independent readers (a senior radiology resident and practicing academic neuroradiologist) for visually apparent PCA territory pCASL hypoperfusion relative to other vascular territories. The pCASL-CBF perfusion imaging protocol consisted of the GE product pCASL sequence (General Electric, Milwaukee, WI) using a 1.5s labeling duration and 2s post-labeling delay (PLD), adapted from white-paper recommendations (1).RESULTS
The fifty unilateral fetal PCA patients ranged from 25 to 93 in age, 17 male and 33 female. Both readers identified eight cases out of the fifty (16%) that had visually apparent hypoperfusion in the PCA territory contralateral to the side of the fetal PCA. Agreement between readers was perfect (100%, κ=1) In all 8 cases, the PCA territory perfusion signal ipsilateral to the fetal PCA qualitatively matched the perfusion signal of the ipsilateral anterior circulation, while the contralateral PCA territory appeared relatively decreased to the other major vascular territories. None of the 8 cases showed PCA territory infarction on DWI/FLAIR, increased oxygen extraction on SWI, or focal neurological symptoms referable to the PCA territory that would explain a true perfusion abnormality.DISCUSSION
Visually-apparent PCA territory hypoperfusion on pCASL perfusion imaging is not uncommon in patients with a contralateral fetal PCA who have no clinical or conventional imaging findings referable to the territory to suggest true hypoperfusion. This apparent hypoperfusion is almost certainly artifactual, secondary to a longer arterial transit time of the ASL label to the non-fetal PCA territory, given a lower blood velocity in the supplying vertebral arteries compared to the higher-velocity ICA supplying the fetal PCA territory. Consequently, at a PLD of 2s (at which time imaging begins), less label has been delivered to the non-fetal side resulting in apparent hypoperfusion. Additionally, since the fetal-PCA territory is supplied by the ICA, it has a similar qualitative appearance to the ipsilateral ACA and MCA territories, which makes the apparent contralateral PCA territory hypoperfusion even more conspicuous.CONCLUSION
Variation in circle-of-Willis anatomy can periodically result in artifactual pCASL perfusion deficits, as highlighted by apparent qualitative PCA hypoperfusion in patients with a unilateral fetal PCA. While quantitative differences in pCASL-CBF due to this phenomenon have been previously described (2), this is the first study to evaluate the frequency of qualitative PCA hypoperfusion in a clinical population with fetal-type PCA anatomy, but without clinical/imaging deficits. It is important for radiologists to be aware that hypoperfusion may arise from variant circle of Willis anatomy, which should not be incorrectly interpreted as reduced perfusion. The use of longer PLD times and/or velocity-based ASL approaches (3) may correct this asymmetry and is an area of future research.Acknowledgements
No acknowledgement found.References
- Alsop DC, Detre JA, Golay X, et al. Recommended implementation of arterial spin-labeled perfusion MRI for clinical applications: A consensus of the ISMRM perfusion study group and the European consortium for ASL in dementia. Magn Reson Med. 2015;73(1):102-16.
- Barkeij Wolf JJH, Foster-Dingley JC, Moonen JEF, et al. Unilateral fetal-type circle of Willis anatomy causes right-left asymmetry in cerebral blood flow with pseudo-continuous arterial spin labeling: A limitation of arterial spin labeling-based cerebral blood flow measurements?. J Cereb Blood Flow Metab. 2016;36(9):1570-8.
- Wong EC, Cronin M, Wu W-C, Inglis B, Frank LR, Liu TT. Velocity-selective arterial spin labeling. Magn Reson Med. 2006;55(6):1334–41.