1617
Differences of Wall shear stress between patients with high-risk and low-risk plaque in carotid artery: A 4D flow MRI study.
Guiling Zhang1, Zhenxiong Wang1, Weiyin Vivian Liu2, and Wenzhen Zhu1
1Tongji hospital, Wuhan, China, 2MR Research, GE Healthcare, Beijing, China
1Tongji hospital, Wuhan, China, 2MR Research, GE Healthcare, Beijing, China
Synopsis
High risk plaque is the is the predominant risk factor of stroke. Accurate diagnosis and intervention could prevent patients from cerebrovascular events. Axial, circumferential and 3D wall shear stress calculated by 4D flow MRI were utilized to explore the difference between high risk plaque patients and low risk plaque patients. The results demonstrated the WSS were all significant higher in high risk plaque group. Our results may provide crucial clues to therapeutic interventions.
Introduction
High-risk plaque characterized by easily rupturing and leading to thrombosis or embolism, is the predominant risk factor of cerebrovascular events1. Low-risk plaque needs conservative treatments like pharmacological interventions while high-risk plaque needs more active treatments like stent placement or endovascular thrombectomy. Therefore, to identify whether the plaque is a high-risk plaque is important. The current definition of high risk plaque is based on pathology, such as intraplaque hemorrhage, lipid core, inflammatory response2. Imaging research on plaque can be generally classified into morphology and hemodynamics. Recently, morphological research has made a breakthrough with the development of high resolution vessel wall imaging (HRVWI), but hemodynamic research is still controversial and requires more research to confirm the vulnerable plaques. In this study, the combination of HRVMI and 4D flow MRI was used to explore the differences of wall shear stress (WSS) between high-risk and low-risk plaques and to identify whether WSS is a predictor of high-risk plaques and provide evidences for further clinical treatment.Method
Forty-four patients with carotid sinus plaques were retrospectively enrolled in the study. All patients underwent CTA, HRVW, and 4D flow MRI. Twenty-eight patients with high-risk plaques and sixteen patients with low-risk plaques. High-risk plaque was defined as (1) no calcification seen on CT images; (2) the signal intensity in the plaque on HRVWIs is not homogeneous and enhanced significantly; (3) cerebrovascular events occurred in the ipsilateral brain parenchyma. Low risk plaque was defined as (1)calcification seen on CT images; (2) the signal intensity in the plaque on HRVWIs is not homogeneous and no enhancement; (3) no cerebrovascular events in the ipsilateral brain parenchyma. The stenosis rate of all plaques was 20%-50% (diagnosis based on HRVWI). 4D Flow MRI data were imported into post-processing software (Version 5.6.6, Circle Cardiovascular Imaging, Canada) to calculate volume (max, mean, min), axial WSS (max, mean, min), circumferential WSS (max, mean, min) and 3D WSS (max, mean, min).Result
Table 1 displayed the demographics characteristics of patients with high-risk and low-risk plaque. The high-risk group showed significantly higher hypertension rate compared to the low-risk group. No significant differences in age, gender, height, weight, diabetes, drinking, smoking, hyperlipidemia and stenosed rate were found between groups. Volume: No difference of blood volume (max, mean, min) between two groups was found (Figure1d).WSS: The axial, circumferential, and 3D WSS were all significantly higher in the high-risk plaque group than the low-risk group except for the minimum axial and circumferential WSS (Figure1a,b,c). Figure 2 showed the WSS distribution of one case in each group.
Discussion
WSS played an important role in the formation and development of atherosclerosis. In our study, WSS discrepancy calculated by 4D flow was still found between two groups when patients with similar stenosis degree confirmed by no difference of vascular volume measurements. Previous studies found that ulcer appeared exclusively at the high-WSS location and higher maximum WSS was also significantly associated with the presence of intraplaque hemorrhage3,4. Gijsen et al. has reported a plaque in the high-WSS region increases strain over time, indicating that lipid deposition likely increases in high WSS5. These aforementioned studies were consitent with ours, but more details such as axial, circumferential and 3D WSS were shown in our study. Only comparisons of the minimum circumferential and axial WSS were significant different, and it should be further confirmed that high WSS was more likely to cause high risk plaque. WSS might affect the function of vascular endothelial and smooth muscle cells, and high WSS even induces specific changes in endothelial cell behavior, including modifying gene expression and expression of matrix metalloproteinases, which may contribute to the initialization and progression of atherosclerosis6-8.Conclusion
Higher WSS was found in patients with high-risk plaque than those with low-risk and may be related to atherosclerotic plaque rupture and cause thrombosis or embolism, leading to cerebrovascular events.Acknowledgements
Supported by the Key Program National Natural Science Foundation of China (Grant No. 81730049)References
1. Falk E, Nakano M, Bentzon JF, Finn AV, Virmani R. Update on acute coronary syndromes: the pathologists view. Eur Heart J 2013;34(10):719-+. doi: 10.1093/eurheartj/ehs411 2. Adamson PD, Dweck MR, Newby DE. The vulnerable atherosclerotic plaque: in vivo identification and potential therapeutic avenues. Heart 2015;101(21):1755-1766. doi: 10.1136/heartjnl-2014-307099 3. Groen HC, Gijsen FJ, van der Lugt A, Ferguson MS, Hatsukami TS, van der Steen AF, Yuan C, Wentzel JJ. Plaque rupture in the carotid artery is localized at the high shear stress region: a case report. Stroke 2007;38(8):2379-2381. doi: 10.1161/STROKEAHA.107.484766 4. Tuenter A, Selwaness M, Lorza AA, Schuurbiers JCH, Speelman L, Cibis M, van der Lugt A, de Bruijne M, van der Steen AFW, Franco OH, Vernooij MW, Wentzel JJ. High shear stress relates to intraplaque haemorrhage in asymptomatic carotid plaques. Atherosclerosis 2016;251:348-354. doi: 10.1016/j.atherosclerosis.2016.05.018 5. Gijsen FJH, Mastik F, Schaar JA, Schuurbiers JCH, van der Giessen WJ, de Feyter PJ, Serruys PW, van der Steen AFW, Wentzel JJ. High shear stress induces a strain increase in human coronary plaques over a 6-month period. Eurointervention 2011;7(1):121-127. doi: 10.4244/Eijv7i1a20 6. Castier Y, Brandes RP, Leseche G, Tedgui A, Lehoux S. p47phox-dependent NADPH oxidase regulates flow-induced vascular remodeling. Circ Res 2005;97(6):533-540. doi: 10.1161/01.RES.0000181759.63239.21 7. Eshtehardi P, Brown AJ, Bhargava A, Costopoulos C, Hung OY, Corban MT, Hosseini H, Gogas BD, Giddens DP, Samady H. High wall shear stress and high-risk plaque: an emerging concept. Int J Cardiovasc Imaging 2017;33(7):1089-1099. doi: 10.1007/s10554-016-1055-1 8. White SJ, Hayes EM, Lehoux S, Jeremy JY, Horrevoets AJ, Newby AC. Characterization of the differential response of endothelial cells exposed to normal and elevated laminar shear stress. J Cell Physiol 2011;226(11):2841-2848. doi: 10.1002/jcp.22629Figures

Table1:
Demographics and clinical features in two groups
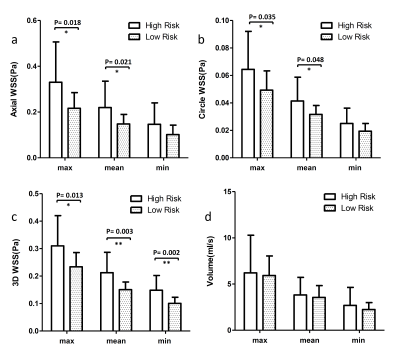
Figure 1: Axial, circumferential
and 3D of WSS as well as volume in high-risk group
and low-risk group. (*P<0.05, **P<0.01)
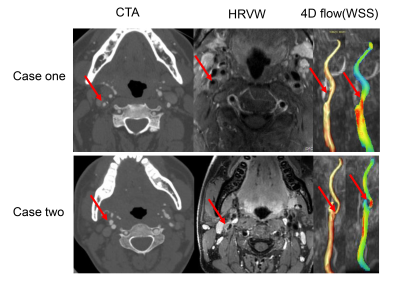
Figure 2 : WSS distribution of one case in representation of low-risk-plaque and
high-risk-plaque group. Case one is a patient with low-risk plaque. Spotted
calcification, eccentric wall thickening with homogenization and no enhancement in HRVM. WSS increased and was higher in the center zone than the
peripheral zone, but overall was lower than case two. Case two is a patient
with high-risk plaque. No calcification was visible, but eccentric wall
thickening with significant enhancement was observed. WSS increased significantly compared to normal controls.