1616
Characteristics of Intracranial Artery Dissection on High-resolution MRI Associated with Recurrent Stroke/Transient Ischemic Attack1Radiology, Changhai hospital of Shanghai, Shanghai, China, 2Changhai hospital of Shanghai, Shanghai, China
Synopsis
HR-MRI is helpful for the classification of IAD, could be used to identify the culprit IAD from non-culprit ones.
Propose
This study aims to identify the HR-MRI features between culprit and non-culprit intracranial artery dissection(IAD) and investigate the clinical and radiological features of different types of IAD.Methods:
In this retrospective study, 101 patients with IAD confirmed by HR-MRI in Changhai Hospital of Shanghai were recruited between January 2014 and January 2019. All patients had normal neurological symptoms within 30 days such as dizziness or headache who underwent the intervention treatment using digital subtraction angiography (DSA), while the part of them had classical cerebral vascular symptoms. Each detected dissection was independently classified as a culprit dissection if a hyperintense lesion was found on DWI in the vascular territory supplied by the branches distal to the site of the dissection with accompanying cerebral vascular symptoms. For each patient, the following data from the HRMRI examinations were recorded: (1) the location of intracranial dissected vessels; (2) the shape of lumen; (3) presence or absence of intramural hematoma; (4) the signal of intramural hematoma; (5) presence or absence of a double lumen; (6) presence or absence of intimal flap; (7) presence or absence of intraluminal thrombus enhancement; (8) presence or absence of intimal flap enhancement; (9) the grade of vessel wall enhancement; (10) the type of the dissection. Univariate analysis was firstly performed by t-tests or Mann-Whitney U test. Multivariate logistic regression analysis was then performed which included the variables that had p<0.10 in the univariate tests.Results:
75 symptomatic patients (mean age: 551.16±12.91 years; 62 males and 13 females) were recruited in the final analysis, including 65 patients with culprit dissection and 20 patients with non-culprit dissection. As it shown in culprit dissection, the two clinical features [age (OR, 0.831; 95% CI, 0.752-0.919; P < 0.001) and hypertension (OR, 66.620; 95% CI, 5.909-751.108; P = 0.001) ] and one HR-MRI feature [intramural hematoma (OR, 16.803; 95% CI, 1.006-280.806; P = 0.037)] were significantly associated with the culprit dissection, and the AUCs of the ROC curves were 0.757, 0.639 and 0.641, respectively. And there were five types of intracranial dissection including classical dissection (N=50), fusiform aneurysm (N=1), long dissected aneurysm (N=3), huge aneurysm (N=9) and cysitical aneurysm (N=12). Age stage (P = 0.042), diabetes (P = 0.010), DSA (P = 0.021), clinical symptoms (P = 0.037), location (P = 0.009), lumen (P < 0.001), and intramural hematoma signal (P = 0.006)were significant predictors to identify the intracranial dissection.Conclusion:
In this study, HR-MRI, which is helpful for the classification of IAD, could be used to both identify the culprit IAD from non-culprit ones and distinguish the characteristics of the IAD unconfirmed by DSA.Discussion
This study investigated the high-risk predictors between culprit and non-culprit dissection in symptomatic patients with IAD and the clinical and radiological features on the IAD unconfirmed by DSA. We found that two clinical features (age and hypertension) and one HR-MRI feature (intramural hematoma) were significantly associated with the culprit dissection while smoking, LDL, location and grade of vessel wall enhancement were significant predictors to identify IAD which hadn’t been confirmed by the gold standard. In addition, we found that HR-MRI could be used to differentiate the types of IAD. Our findings indicate that HR-MRI examinations of intracranial arteries may provide additional information for risk stratification in predicting and identifying IAD compared with the clinical symptoms. As previous study reported, more than 70% of patients with cervicocerebral artery dissection presented with ischemic stroke, and it accounts for approximately 15% of ischemic strokes in young patients (15–49 years old). Similarly, in our study, we found that the younger the patients with IAD were (29.3% of patients with culprit dissection were less than 45 years old), the more recent neurological symptoms they have. What’s more, another factor associated with symptomatic IAD is hypertension as shown in this study, which was also prevalent in young adults with a 4-11% increase over the past decade.Shin et.al described that there was a higher prevalence of hypertension in patients with IAD than those with cervical artery dissection. A recent research indicated that hypertension was an important predicting factor associated with ischemic stroke in the whole cohort of patients with vertebral artery dissection on univariate logistics regression.Acknowledgements
NoneReferences
[1] Uemura M, Terajima K, Suzuki Y, et al. Visualization of the Intimal Flap in Intracranial Arterial Dissection Using High-Resolution 3T MRI. J Neuroimaging. 2017 Jan;27(1):29-32.
[2] Jung SC, Kim HS, Choi CG, et al. Quantitative Analysis Using High-Resolution 3T MRI in Acute Intracranial Artery Dissection.J Neuroimaging. 2016 Nov;26(6):612-617.
[3] Coppenrath E, Lenz O, Sommer N, et al. Clinical Significance of Intraluminal Contrast Enhancement in Patients with Spontaneous Cervical Artery Dissection: A Black-Blood MRI Study. Rofo. 2017 Jul;189(7):624-631.
[4] Jensen MB, Chacon MR, Aleu A. Cervicocerebral arterial dissection. Neurologist. 2008;14:5-6 10.
[5] Ortiz J, Ruland S. Cervicocerebral artery dissection. Curr Opin Cardiol. 2015;30:603-610.
[6] Ekker MS, Boot EM, Singhal AB, Tan KS, Debette S, Tuladhar AM, et al. Epidemiology, aetiology, and management of ischaemic stroke in young adults. Lancet Neurol. 2018;17:790-801.
[7] Wu Y, Wu F, Liu Y, Fan Z, Fisher M, Li D, et al. High-resolution magnetic resonance imaging of cervicocranial artery dissection: Imaging features associated with stroke. Stroke. 2019;50:3101-3107.
[8]Shin DH, Hong JM, Lee JS, Nasim R, Sohn SI, Kim SJ, et al. Comparison of potential risks between intracranial and extracranial vertebral artery dissections. Eur Neurol. 2014;71:305-312.
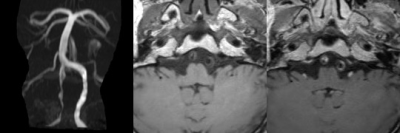
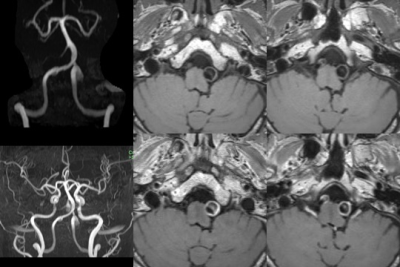
Figures