1614
Plaque characteristics and implication on mechanism in border-zone infarction caused by middle cerebral artery atherosclerosis1Radiology, Tianjin First Central Hospital, tianjin, China, 2BIRI, Cedars-Sinai Medical Center, Los Angeles, CA, United States, 3Neurology, Tianjin First Central Hospital, tianjin, China
Synopsis
This study aimed to investigate atherosclerotic plaque characteristics in middle cerebral artery (MCA) atherosclerotic patients with border-zone (BZ) infarction using magnetic resonance vessel wall imaging (MR-VWI). In 84 retrospectively enrolled ischemic stroke patients caused by MCA atherosclerosis, the characteristics of culprit plaques were quantitatively compared between BZ only infarction and combined border-zone and pial (BZ+PI) infarction groups. BZ+PI infarction was associated with a higher degree of stenosis and higher plaque-wall contrast ratio and enhancement ratio, compared with BZ only infarction, suggesting that embolic pathogenesis may also account for BZ+PI infarction in addition to hemodynamic compromise.
Introduction
Border-zone (BZ) infarction is a common form of ischemic strokes1. Determination of the mechanism for BZ infarction may have considerable impact on primary and secondary prevention strategies. Previous studies of BZ infarction have relied mainly on routine neuroimaging and focused on internal carotid artery disease2. The mechanisms of BZ infarction in patients with middle cerebral artery (MCA) atherosclerotic disease remain unclear. It has long been debated whether BZ infarction is caused by stenosis-induced hemodynamic compromise or by embolisms3. MR vessel wall imaging (VWI) has emerged as a non-invasive modality that can directly characterize intracranial atherosclerotic plaques4. The present study aimed to use this tool to investigate the mechanism for BZ infarction caused by MCA atherosclerosis.Methods
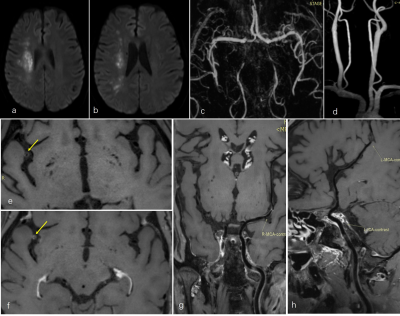
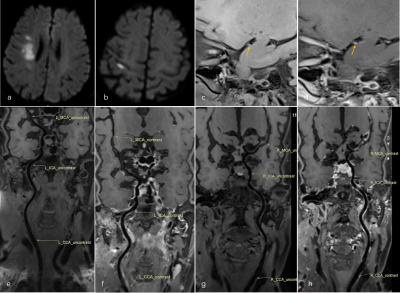
The local institutional review board approved this study. Patients who received both routine brain MR and MR-VWI from October 2016 to January 2019 (56 males; range: 41– 75years) were retrospectively reviewed and those presenting with acute BZ infarction caused by middle cerebral artery atherosclerosis were included in analysis. All MR studies were performed on a 3.0T MR Siemen (MAGNETOM Trio or Prisma, Siemens Healthineers, Erlangen, Germany). Imaging protocol included T1-weighted imaging, T2-weighted imaging, diffusion weighted imaging (DWI), MR angiography (MRA) and pre- and post-contrast MR-VWI using a 3D T1-weighted whole-brain sequence5,6. The major imaging parameters of MR-VWI were: TR/TE = 900/14 msec; acquisition matrix size = 384×300; field of view = 210×164 mm2; resolution = 0.55 × 0.55 × 0.55 mm; pixel bandwidth = 465 Hz/pixel; scan time = 8 minutes.DWI lesion patterns were analyzed by a neuroradiologist blinded to clinical data. The topography of acute ischemic lesions was determined using published templates. The vascular territories were divided into perforator, pial, and border zones, and brain infarction was accordingly classified as perforating artery infarction (PAI), pial infarction (PI) and border-zone (BZ) infarction7. BZ infarction is further divided into internal border-zone (IBZ) and external border-zone (EBZ) infarction. The culprit atherosclerotic lesion at the MCA was determined in consensus by a neurologist and neuroradiologist. The characteristics of the culprit MCA plaques were compared between BZ-only infarction and BZ+PI infarction groups and compared between IBZ infarction and EBZ infarction groups. Following plaque features were assessed on cross-sectional views of individual lesions: degree of stenosis, plaque length, plaque-wall contrast ratio, and plaque contrast enhancement ratio.
Results
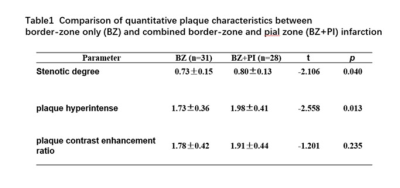
A total of 59 patients were included in analysis, including 31 BZ-only infarctions and 28 combined BZ and PI infarctions (BZ+PI). Compared with the BZ-only infarction patients, BZ+PI infarction patients had significantly higher degree of stenosis (P =0.040) and plaque-wall contrast ratio (P=0.013). There were no significant differences in plaque length and plaque contrast enhancement ratio between the two groups. We identified 19 patients with IBZ (61.3%), 8 with EBZ (25.8%) and 4 with both IBZ and EBZ (12.9%) in the BZ-only group. There were no significant differences in degree of stenosis, plaque-wall contrast ratio, and plaque contrast enhancement ratio between IBZ and EBZ groups. Patients with EBZ were more likely to have higher degree of stenosis than those with IBZ, although the difference was not significant (P=0.058).Discussion and conclusion
BZ+PI infarction was associated with higher degree of stenosis and plaque-wall contrast ratio, compared with BZ-only infarction. High plaque-wall contrast ratio has been considered a risk factor for plaque vulnerability8. Hence, it can be conjectured that embolic pathogenesis may also account for BZ+PI infarction in addition to hemodynamic compromise. IBZ infarction is more common in BZ infarction patients caused by MCA arteriosclerosis. However, there was clear evidence regarding the role of hemodynamic compromise and embolic pathogenesis in causing IBZ and EBZ. Investigation of other plaque aspects may be warranted. MR-VWI may serve as a useful tool to provide insights into BZ infarction mechanisms.Acknowledgements
No acknowledgement found.References
1 R Mangla, B Kolar, J Almast, SE Ekholm. Border zone infarcts: pathophysiologic and imaging characteristics. RadioGraphics 2011; 31:1201–1214.
2 Moustafa RR, Izquierdo-Garcia D, Jones PS,et al. Watershed Infarcts in Transient Ischemic Attack/Minor Stroke With >50% Carotid Stenosis Hemodynamic or Embolic? Stroke. 2010;41:1410-1416.
3 El-Gammal TM, Bahnasy WS, Ragab OAA, Al-Malt AM. Cerebral border zone infarction: an etiological study. Egypt J Neurol Psychiatr Neurosurg. 2018;54(1):6.
4 JD Bodle, E Feldmann, RH Swartz, et al. High-Resolution Magnetic Resonance Imaging An Emerging Tool for Evaluating Intracranial Arterial Disease. Stroke. 2013;44:287-292.
5 Fan Z, Yang Q, Deng Z, et al. Whole-brain intracranial vessel wall imaging at 3 Tesla using cerebrospinal fluid-attenuated T1-weighted 3D turbo spin-echo. Magnetic Resonance in Medicine 2017;77: 1142-1150.
6 Q Yang, Z Deng, X Bi,et al. Whole‐brain vessel wall MRI: A parameter tune‐up solution to improve the scan efficiency of three‐dimensional variable flip‐angle turbo spin‐echo. JMRI 2017;46:751-757.
7 DK Lee, JS Kim, SU Kwon, et al. Lesion Patterns and Stroke Mechanism in Atherosclerotic Middle Cerebral Artery Disease Early Diffusion-Weighted Imaging Study. Stroke. 2005;36:2583-2588.
8 Wu F, Ma Q, Song H, et al. Differential features of culprit intracranial atherosclerotic lesions: a whole-brain vessel wall imaging study in acute ischemic stroke patients. Journal of the American Heart Association 2018;7:e009705.
Figures