1609
Evaluating cervical artery dissections in young adults - A Comparison Study between High-Resolution MRI and CT Angiography1Department of Radiology, Shandong Provincial Hospital Affiliated to Shandong University, Jinan, China, 2Department of Vascular Surgery, Shandong Provincial Hospital Affiliated to Shandong University, Jinan, China, 3MR Scientific Marketing, Diagnosis Imaging, Siemens Healthcare Ltd, Beijing, China
Synopsis
This study aimed to compare the diagnostic values between HR-MRI and CTA in young adults with cervical artery dissections. Totally 42 patients with ischemic stroke were recruited, including 20 carotid artery dissections, 12 vertebral artery dissections and 10 non-dissected cervical arteries. Two radiologists separately analyzed all the images. According to the radiologists’ scores for the likelihood of the dissections, positive predictive value, negative predictive value, sensitivity and specificity for both modalities were calculated. We found the higher sensitivity and specificity of HR-MRI. This study supports the value of HR-MRI in non-invasive diagnosis of young adults due to cervical artery dissections.
Purpose
Stoke remains the competing risk of demise and the leading cause of disability from other causes for the patients, such as cancer and infectious diseases.1 The estimated global lifetime risk of stroke for the age between 18 years and 45 years is relatively high among the population. Cervical-artery dissection is the major cause of ischemic stroke in young adults. The purpose of this study is to compare the application and diagnosis performance of high-resolution magnetic resonance (HR-MRI) with computed tomographic angiography (CTA) on young patients with ischemic stroke due to cervical artery dissections.Material and Methods
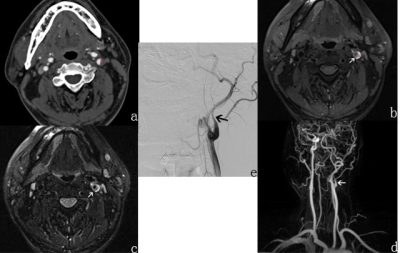
Totally 42 symptomatic patients were involved in this retrospective study. Among them, 38 patients underwent CTA, HR-MRI and Digital Subtraction Angiography (DSA) for diagnosis, while the remaining 4 patients of vertebral artery dissections were diagnosed by follow-up after 2-3 month therapy (anticoagulant therapy and symptomatic treatment).The MRI examinations were performed on a 3T whole body scanner (MAGNETOM Verio, Siemens Healthcare, Erlangen, Germany) with a standard 16-channel head-neck coil. The HR-MRI protocol contains a 3D time of flight (TOF) sequence with the following parameters: repetition time (TR) = 20 ms, echo time (TE) = 3.27 ms, field-of-view (FOV) = 230mm × 195mm, slice thickness = 1 mm, axial orientation, covering from the carotid bifurcation to wills circle. The 2D T1-weighted fat saturated (fs) dark blood (db) turbo spin echo (TSE) was scanned in transversal plane with the parameters of TR = 1000ms, TE = 26ms, FOV = 140mm × 140mm, matrix = 256 × 256, slice thickness = 2mm, 14 slices, covering the dissection part. The 2D T2-weighted fs-db-TSE was applied with TR = 2500ms, TE = 60ms, FOV = 140mm × 140mm, matrix = 256 × 256, slice thickness = 2mm, 14 slices. Gd-DTPA was used for contrast enhancement (CE) via vessel injection, with the bolus of 0.2 ml/kg (total bolus 10-15ml). The non-CE and CE 3D T1-weighted SPACE was used in sagittal plane, with the sequence parameters of TR = 700ms, TE = 20ms, FOV = 241mm × 241mm, matrix = 256 × 256, slice thickness = 0.9mm, 128 slices, covering from carotid bifurcation to wills circle.
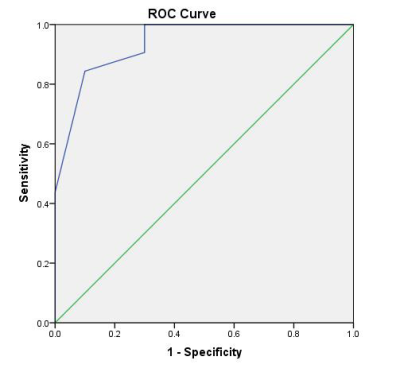
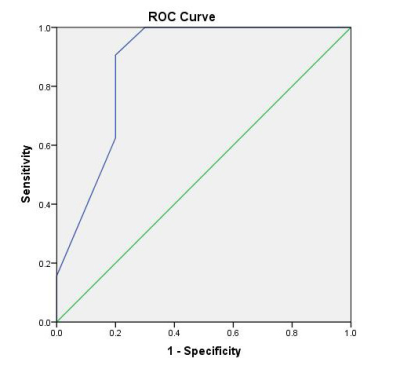
CTA examination was performed on a 320-slice CT scanner (Aquillion ONE, Toshiba Medical Systems, Japan) with high-pitch spiral scan mode. CTA and HR-MRI images were separately and blindly analyzed by two radiologists. The diagnosis performance of HR-MRI and CTA was examined, including sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV). The receiver operating characteristic (ROC) curves for the likelihood of diagnosis of the dissections were analyzed, and their corresponding area under the curve (AUC) of each imaging modality was calculated.
Results
A total of 20 carotid artery dissections, 12 vertebral artery dissections and 10 non-dissected cervical arteries were detected by both HR-MRI and CTA. The inter-observer concordance of HR-MRI and CTA was moderate (κ = 0.806 vs. 0.776). The sensitivity and specificity of HR-MRI and CTA on detecting the dissections are 87.5% vs. 62.5%, and 90.0% vs. 80.0%, respectively. Area under the ROC curve of HR-MRI (0.94 [95% CI, 0.86–0.97]) was greater than that of CTA (0.87 [95% CI, 0.71–1.0]).Discussion
Cervical artery dissections often manifested as mural hematoma. The signal intensity of an acute hematoma within the first 48 hours is hypointense on T1WI and T2WI. Between one week and two months, intramural hematoma will show hyper-intensity on T1-weighted images. And subacute intramural hematomas have a characteristic crescent shape with hyper-intensity around of the vessel lumen.2,3However, if the intramural hematoma surrounding the lumen in subacute or chronic cerebral infarction, it manifested as equidensity or low density on CTA, which may cause missed diagnosis as luminal stenosis or occlusions and misdiagnosis with atypical atherosclerosis, Takayasu Arteritis or other diseases. Most patients in this study had sub-acute or chronic cerebral infarction, which might explain the results of this study that the sensitivity and specificity of HR-MRI is relatively higher.In some cases of this study, the signal intensity of the hematoma in HR-MRI was complex and the form of the hematoma did not manifest as crescent shape around of the vessel lumen. However, we could not find other typical signs. Thus, we need to perform a further study and explore more signs to accurate diagnosis.
Conclusions
Compared to CTA, HR-MRI is more sensitive and specific for the diagnosis of cervical artery dissections in high-risk symptomatic patients. This study supports the value of HR-MRI in non-invasive diagnosis of young adults with cervical artery dissections.Acknowledgements
No acknowledgement found.References
1. Maigeng Zhou, Haidong Wang, Xinying Zeng, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2019; 394:1145-1158.
2. Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol 2009; 8:668-678.
3. Flis CM, Jäger HR, Sidhu PS. Carotid and vertebral artery dissections: clinical aspects, imaging features and endovascular treatment. Eur Radiol 2007; 17:820-834.
Figures