1603
3D-CUBE T1 vessel wall imaging and Susceptibility Weighted Imaging in the diagnosis of cerebral venous sinus thrombosis: a comparison study1Department of Radiology, Qilu Children's Hospital of Shandong University, Jinan, China, 2GE Healthcare, MRI Research China, Beijing, China, 3Shandong Province Qianfoshan Hospital, Jinan, China
Synopsis
This study was aimed at investigating the clinical value of CUBE MRI for high resolution imaging and susceptibility weighted imaging (SWI) in the diagnosis of cerebral venous sinus thrombosis (CVST). The sensitivity, specificity, positive predictive value, and negative predictive value for 3D-CUBE T1 and SWI were calculated respectively. In this study, the diagnosis results of T1 weighted CUBE were better than that of SWI in comparison with the referential diagnosis in the detection of CVST. We therefore demonstrated that the T1 weighted CUBE MRI provided more effective usefulness than SWI in the diagnosis efficacy of the CVST.
Introduction
Cerebral venous sinus thrombosis (CVST), as an uncommon form of stroke, has been difficult diagnosed because of its low incidence and diverse clinical manifestation1. The current preferred method is the combination of magnetic resonance imaging (MRI) to visualize the thrombi in the dural sinuses and magnetic resonance venography (MRV) to detect the filling defects of the corresponding vessels. Given the variation in venous anatomy and the phenomenon of flow gaps, it is sometimes impossible to exclude CVST on MRV2. This study was aimed at evaluating the clinical value of 3D-CUBE T1 vessel wall imaging and susceptibility weighted imaging (SWI) in the diagnosis of CVST.Materials and Methods
Subjects30 consecutive patients (mean age: 42.0±6.4 years old), clinically suspected as CVST by neurology department in the Shandong Province Qianfoshan Hospital from March 2016 to September 2017, were prospectively recruited in this study. The clinical stage was considered acute if the duration of symptoms was ≤3 days, subacute if it was 4-14 days, and chronic if it was ≥15 days3.
Each patient was measured with multiple MR imaging sequences, including plain scan, MRV, SWI and 3D-CUBE T1 vessel wall imaging. Written informed consents were obtained from each patient.
MRI Experiments
All experiments were performed on a 3T clinical scanner (Discovery 750w, GE Healthcare, USA) equipped with a 32-channel head coil.
MRV imaging was firstly acquired with the following scan parameters of repetition time (TR) = 15.8 ms, echo time (TE) = 4.3 ms, thickness = 2 mm, gap = 1 mm, matrix size = 352 *192.
3D CUBE T1 weighted sequence was scanned with scan parameters of TR = 600 ms, TE = 14.4 ms, thickness = 1 mm, gap = 0.5 mm, FOV = 200 mm * 200 mm for whole brain coverage, matrix size = 288 * 288. Total scanning time was 4 minutes 16s.
For SWI measurement, the applied scan parameters included TR = 76.8 ms, TE = 42.8 ms, thickness = 2 mm, gap = 1 mm, flip angle = 15o, matrix size = 350 * 256.
Data analysis
The reference MRI standard of CVST diagnosis was based on the combination of plain scan and MRV because they were the recommended protocol for CVST diagnoses1. The following 8 venous segments were evaluated for each of the patient: superior sagittal sinus, inferior sagittal sinus, left transverse sinus, right transverse sinus, left sigmoid sinus, right sigmoid sinus, straight sinus, confluence of sinus. Two kinds of image datasets including 3D-CUBE T1 and SWI were analyzed respectively by two experienced neuroradiologists who were blinded to the patient information, the other imaging tests and the referential diagnosis. For 3D-CUBE T1, the diagnosis of CVST was based on the isointense/hyperintense lesions relative to the brain parenchyma on the dural sinuses. SWI for detecting CVST was defined as the presence of hypointensity within the dilated dural sinuses.
MedCalc 15.2.2 (MedCalc, Mariakerke, Belgium) was used to perfomed the analysis. By the referential diagnostic criteria of CVST, evaluated the accuracy of 3D-CUBE T1 and SWI on per patient and per segment level by respectively calculating their sensitivity, specificity, positive predictive value, negative predictive value, and the area under the ROC curve.Agreements for 3D-CUBE T1 and SWI with reference diagnosis were examined by using the kappa coefficient agreement. The level of statistical significance was set at P<0.05.
Results
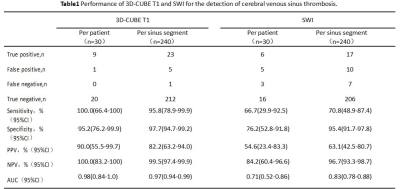
The final referential diagnosis of the CVST was for 24 venous sinus segments in 9 patients. The median time between disease onset and MRI measurements was 18.8 days within a range from 6 to 45 days.Using ROC analysis, the sensibility/specificity for 3D-CUBE imaging were 100%/95.2% per patient and 95.8%/97.7% per sinus segment, with the area under the ROC curve being 0.98 per patient and 0.97 per sinus segment, respectively (Table 1). In comparison, the sensibility/specificity for SWI were 66.7%/76.2% per patient and 70.8%/95.4% per sinus segment, with the area under the ROC curve being 0.71 per patient and 0.83 per sinus segment, respectively (Table 1). The AUC based on patient and sinus segment for 3D-CUBE imaging were significant higher than that of SWI (P<0.05). The agreement bewteen 3D-CUBE imaging and reference diagnosis was better, by the value of k were 0.923 based on patient and 0.871 based on segment.
Disscussion and conclusion
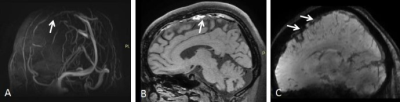
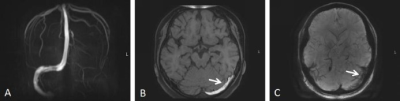
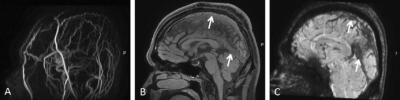
In this study, 3D-CUBE imaging showed better accuracy, especially in transverse and sigmoid sinuses where the surrounding low signal intensity of air or bone could affect the diagnosis of thrombi in SWI. For the identification of intraluminal thrombi, we found that 3D-CUBE imaging showed the thrombi staging as evident hyperdensity in the clinical subacute stage(Figure 1,2), isodensity in the clinical chronic stage(Figure 3). Other studies have also found that 3D black blood sequence was useful in the diagnosis of subacute cerebral venous thrombus4. However, SWI showed the hypodensity thrombi in both subacute and chronic stages.In conclusion, 3D-CUBE imaging can be used to diagnose CVST with higher sensibility and specificity compared with SWI. Therefore, CUBE imaging can be considered an effective tool in the clinical diagnosis and treatment of CVST.
Acknowledgements
We thank Weiqiang Dou from GE Healthcare for this valuable support on the 3D-CUBE T1 vessel wall sequence.References
1.Bousser M G, Ferro J M. Cerebral venous thrombosis: an update. Lancet Neurol 6:162-170[J]. Lancet Neurology, 2007, 6(2):162-170.
2.Saposnik G, Barinagarrementeria F, Jr B R, et al. Diagnosis and management of cerebral venous thrombosis: a statement for healthcare professionals from the American Heart Association/American Stroke Association[J]. Stroke, 2011, 42(4):1158.
3.Altinkaya N, Demir S, Alkan O, et al. Diagnostic value of T2*-weighted gradient-echo MRI for segmental evaluation in cerebral venous sinus thrombosis[J]. Clinical Imaging, 2014, 39(1).
4.Niu P P, Yu Y, Guo Z N, et al. Diagnosis of non-acute cerebral venous thrombosis with 3D T1-weighted black blood sequence at 3T[J]. Journal of the Neurological Sciences, 2016, 367:46-50.
Figures