1600
Diagnostic feasibility of high resolution vessel wall imaging for isolated posterior inferior cerebellar artery dissection1Radiology, Ajou University Medical Center, Suwon, Republic of Korea
Synopsis
We evaluate the feasibility of HR-VWI for diagnosing PICA dissection. Our results demonstrated that HR-VWI could effectively diagnose arterial dissection even in PICA, small diameter vessel. The dissection flap with outer wall enlargement on T2W HR-VWI was most confident sign for diagnosing PICAD. Isolated PICAD is not a rare cause of ischemic stroke in posterior circulation. Therefore, in case of PICA territory infarction of uncertain origin, differentiating PICAD using HR-VWI is necessary for proper treatment of patients, and T2WI should be included in HR-VWI.
INTRODUCTION
The spontaneous isolated posterior inferior cerebellar artery dissection (PICAD) has been known to be a rare disease entity, especially in case of dissection presented as ischemic stroke.1-4 Recent progress in neuroimaging techniques, high resolution-vessel wall imaging (HR-VWI), have improved diagnosis of arterial dissection, and dissections presented as luminal stenosis and ischemic stroke have been found to be more common than previous thought.5-7 Therefore, the purpose of this study was to clarify the radiologic features of PICAD presented as ischemic stroke and to show the diagnostic feasibility of HR-VWI for PICAD that has been underdiagnosed.METHODS
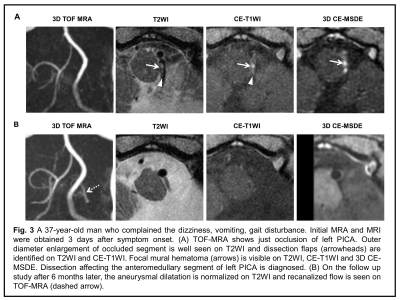
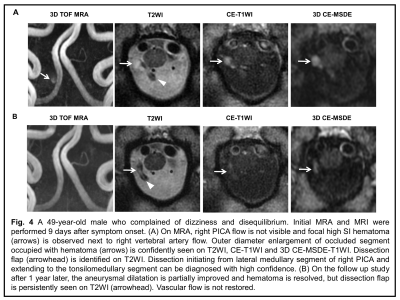
We retrospectively reviewed consecutive 468 patients suspected of having arterial dissection involving posterior cerebral circulation and underwent HR-VWI between March 2012 and July 2019. 309 patients were diagnosed with arterial dissection involving posterior cerebral circulation and 44 patients among them (14.2%) finally diagnosed with isolated PICAD. The confirmative diagnosis was decided by consensus of 3 experts composed with neuroradiologist, neurointerventionist and stroke neurologist after reviewing all clinical and paraclinical investigations (initial CT, MR, DSA images and etiologic work up) available at hospital and follow-up. At least one imaging or clinical follow up was performed within 3 months. The HR-VWI consist of 2D sequences(PD, T2, T1, CE-T1 with FOV of 10cm, matrix size of 200x200, slice thickness of 2mm and black blood imaging using saturation band), 3D contrast enhanced Motion-sensitized driven-equilibrium (CE-MSDE) T1 sequences with voxel size of 1mm and TOF MRA with source images. Two neuroradiologists independently reviewed HR-VWI and looked for direct evidence of dissection (mural hematoma, dissection flap, outer wall dilatation on T2WI of steno-occlusive segment on vascular image) on each sequences of HR-VWI. The visualization of direct evidence was scaled as 0 = not demonstrated, 1 = demonstrated but not clearly visualized, and 2 = clearly visualized. Diagnostic confidence was also scored as 5 point scale; 1 = not suspicious to 5 = definite PICAD. Intra- and inter-observer agreement for diagnosing PICAD and detecting dissection evidences were estimated with weighted kappa coefficientRESULTS
Finally 43 patients (median age: 48years, range: 33-65 years) were enrolled in this study. A patient was excluded, because dissecting segment was not fully covered on HR-VWI. On CTA and MRA, PICAD were most often presented as occlusion (41.9%), in contrast, stenosis and dilatation on DSA (57.7%). Among dissection signs (Table on Fig. 1), dissecting flap were detected on T2WI in all cases of PICAD, most of dissection flaps (83.7%) were also clearly visualized. Outer wall enlargement were also detected in almost of cases (97.7%). The mural hematomas were more frequently observed in CE-T1WI (95.3%) and 3D CE-MSDE-T1WI (97.1%) than in T2WI (76.7%). Mean diagnostic confidence scoring was 4.72. In 38 patients (88.4%), T2WI was the most useful sequence for diagnosing PICAD, CE-T1WI was more useful than T2WI in only 5 patients (11.6%). The intra/inter-observer agreement (Table on Fig. 1) for detecting dissection sign showed more than substantial agreement (0.62~0.94). In diagnostic confidence scoring, almost perfect agreement was observed (intra-/inter-reader agreement, 0.97/0.92)DISCUSSION
The isolated PICAD were diagnosed in 14.2% of arterial dissection involving posterior cerebral circulation in our study, this incidence is higher than that (5.4~9.8%) in previous reports.1,8,9 The diagnosis rate of isolated PICAD presented as ischemic stroke is increasing with the recent progress in vessel wall imaging.Recent reviews 10-12 about HR-VWI for arterial dissection considered the CE 3D T1WI as the most optimal sequence and mural hematoma as the most common finding. However, these studies targeted the vertebrobasilar artery. In cases of PICA, which has smaller diameter than vertebrobasilar artery, T2W HR-VWI seems more helpful for diagnosis of dissection by viewing vessel dilatation. In our study, T2W HR-VWI clearly showed the outer wall dilatation of PICA by the dissection in most of cases (97.7%) and was more useful than CE T1WI, regardless of 2D or 3D. Furthermore, unlike the intramural hematoma which shows active change of signal intensity according to disease stage and is less sensitive in acute stage, dissection flap were clearly visualized in most of our cases (83.7%) on T2W HR-VWI, irrespective of stage. Therefore, to diagnose the PICAD, finding a dissection flap and outer wall dilatation on T2W HR-VWI may be more useful than finding a mural hematoma on T1WI.
The 3D HR-VWI has the advantages, image reformat of various planes and wide field of view. However, our results showed that 2D HR-VWI achieved higher detection rate for dissection evidences. This might be due to the lower spatial resolution of 3D CE-MSDE, voxel size of 1.0 versus 0.5mm for 2D HR-VWI of our protocol. For achieving higher spatial resolution of 3D MSDE-T1WI, 0.5mm voxel size as like 2D T1W HR-VWI, the acquisition time have to be longer, 2 or 3 times. Prolonged acquisition times will inevitably lead to degradation of image quality from the patient’s movement which frequently occurs in patients with dissection due to severe headache, cerebral infarction or subarachnoid hemorrhage
CONCLUSION
The HR-VWI could effectively diagnose arterial dissection even in PICA, small diameter vessel. The dissection flap with outer wall enlargement on T2W HR-VWI was most confident sign for diagnosing PICAD.Acknowledgements
No acknowledgement found.References
1. Matsumoto J., Ogata T., Abe H., et al. Do characteristics of dissection differ between the posterior inferior cerebellar artery and the vertebral artery? J Stroke Cerebrovasc Dis 2014;23(10):2857-2861.
2. Sedat J., Chau Y., Mahagne M. H., et al. Dissection of the posteroinferior cerebellar artery: clinical characteristics and long-term follow-up in five cases. Cerebrovasc Dis 2007;24(2-3):183-190.
3. Tawk R. G., Bendok B. R., Qureshi A. I., et al. Isolated dissections and dissecting aneurysms of the posterior inferior cerebellar artery: topic and literature review. Neurosurg Rev 2003;26(3):180-187.
4. Park M. G., Choi J. H., Yang T. I., et al. Spontaneous isolated posterior inferior cerebellar artery dissection: rare but underdiagnosed cause of ischemic stroke. J Stroke Cerebrovasc Dis 2014;23(7):1865-1870.
5. Choi J. W., Han M., Hong J. M., et al. Feasibility of improved motion-sensitized driven-equilibrium (iMSDE) prepared 3D T1-weighted imaging in the diagnosis of vertebrobasilar artery dissection. J Neuroradiol 2018;45(3):186-191.
6. Park K. J., Jung S. C., Kim H. S., et al. Multi-Contrast High-Resolution Magnetic Resonance Findings of Spontaneous and Unruptured Intracranial Vertebral Artery Dissection: Qualitative and Quantitative Analysis According to Stages. Cerebrovasc Dis 2016;42(1-2):23-31.
7. Han M., Rim N. J., Lee J. S., et al. Feasibility of high-resolution MR imaging for the diagnosis of intracranial vertebrobasilar artery dissection. Eur Radiol 2014;24(12):3017-3024.
8. Kwon J. Y., Kim N. Y., Suh D. C., et al. Intracranial and extracranial arterial dissection presenting with ischemic stroke: Lesion location and stroke mechanism. J Neurol Sci 2015;358(1-2):371-376.
9. Chang F. C., Yong C. S., Huang H. C., et al. Posterior Circulation Ischemic Stroke Caused by Arterial Dissection: Characteristics and Predictors of Poor Outcomes. Cerebrovasc Dis 2015;40(3-4):144-150.
10. Tan H. W., Chen X., Maingard J., et al. Intracranial Vessel Wall Imaging with Magnetic Resonance Imaging: Current Techniques and Applications. World Neurosurg 2018;112:186-198.
11. Mandell D. M., Mossa-Basha M., Qiao Y., et al. Intracranial Vessel Wall MRI: Principles and Expert Consensus Recommendations of the American Society of Neuroradiology. AJNR Am J Neuroradiol 2017;38(2):218-229.
12. Kontzialis Marinos, Wasserman Bruce A. Intracranial vessel wall imaging: current applications and clinical implications. Neurovascular Imaging 2016;2(1):4.