1598
High-resolution MRI of primary and secondary central nervous system vasculitis1Shandong First Medical University & Shandong Academy of Medical Sciences, Jinan, China, 2The First Affiliated Hospital of Shandong First Medical University, Jinan, China, 3GE Healthcare, MR Research, Beijing, China
Synopsis
The main goal of this study was to evaluate the treatment effect of primary angiitis of the central nervous system (PACNS) and secondary central nervous system vasculitis(CNSV) with high-resolution magnetic resonance vascular wall imaging. We measured 4 patients with PACNS and 10 patients with secondary CNSV using high resolution CUBE MRI. We found that high-resolution magnetic resonance vascular wall imaging can assess the treatment effect of PACNS and secondary CNSV. Therefore, CUBE MRI can be considered an effective tool in the evaluation of PACNS and secondary CNSV.
Introduction
Central nervous system vasculitis (CNSV) is a group of diseases characterized by the inflammation and destruction of the vessels.1 According to etiology, it can be divided into the primary angiitis of the central nervous system (PACNS) and secondary CNSV. PACNS is a rare and severe immunoinflammatory disease with complicated etiology,while the secondary CNSV is caused by systemic vasculitis, infectious vasculitis and some other diseases. Large differences have been found in the course and prognosis between these two types of CNSV.2 However, at present, few imaging studies compared the differences of the course and treatment effect of these two types.High-resolution magnetic resonance vascular wall imaging,i.e., CUBE MRI, has shown the potential to diagnose and evaluate the CNSV.3,4,5 However it remains unknown if this technique is feasible to assess CNSV with different severities and to even assess the treatment effect on this disease.
To investigate these, high resolution CUBE MRI has been applied to measure patients with PACNS and secondary CNSV before and after 6 months treatment. The correspondingly acquired CUBE images were analyzed. The resultant in lesions were compared between both groups and also between before and after treatment.
Materials and Methods
Subjects4 patients (mean age:45 ± 7 years old) confirmed with PACNS and 10 patients (mean age: 48 ± 14 years old) confirmed with the secondary CNS vasculitis clinically were recruited in this study for MRI experiments. Written informed consents were obtained from each patient.
MRI experiment
A 3T clinical scanner (Discovery 750w, GE Healthcare, Milwaukee, WI, USA) equipped with a 32channel coil was used in the study. 14 patients were performed using a contrast-enhanced 3D T1-weighted high resolution CUBE imaging for vascular wall imaging before and after 6 months treatment. The corresponding scan parameters include:TR=600ms; TE=14.4ms; slice gap=0.5mm; slice thickness =1mm; FOV = 200×200mm2; NEX=0.5, matrix size=288x288 and echo length train=24. The total scan time was 4 minutes 16 seconds.
Data analysis
To evaluate the difference of vascular wall imaging before and after 6 months treatment, the signal-to-noise ratio (SNR) and contrast-to-noise ratio (CNR) were calculated with the defined equations shown below: SNR= Swall /Snoise [Eq.1]
And, CNR=︱Swall−Slumen︱/SDnoise [Eq.2]
, where, Swall, Slumen and Snoise represent the mean signal intensities of the vessel wall, lumen and background, respectively, and SDnoise is the standard deviation of the noise.
All statistical analyses were performed in SPSS software 24.0. The embedded McNemar-test was used to evaluate the alterations of the vascular wall characteristics, including the degree of enhancement and ring sign between PACNS and secondary CNSV patients. In addition, paired-sample t test was separately applied to estimate the difference of the wall max-thickness, SNR and CNR before and after 6 months treatment. The significant threshold was set as p =0.05.
Results
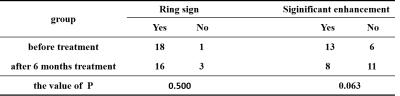
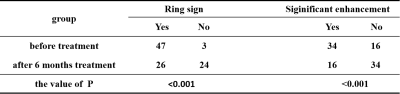
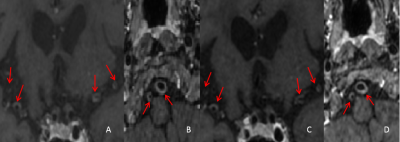
A total of 19 vascular segments were involved in 4 PACNS patients. Compared the vessel images before and after 6 months treatment(Figs.1), no statistical differences were shown in these segments including ring sign and signal intensity enhancement of vascular wall (Table 1), and the wall max-thickness (p>0.05). However, SNR and CNR values of vessel wall imaging have significant difference before and after 6 months treatment (p=0.032, p=0.041). In comparison, there were 50 vascular segments involved in 10 patients with secondary CNSV. Significant differences were found in these segments before and after 6 months treatment in MR appearances including ring sign and signal enhancement of vascular wall (Table 2)(Figs.2). In addition, significant differences were also revealed in the wall max-thickness, SNR and CNR values before and after 6 months treatment (all p<0.001).Discussion
In our study, the vascular walls of both groups showed significant concentric thickening and enhancement before clinical treatment. After 6 months treatment, most of the vascular walls in the PACNS group did not have significant alterations in imaging characteristics and wall max-thickness, and only showed the difference in SNR and CNR. These agreed with the findings previously reported by obusez et al.5 The enhancement of vascular wall of PACNS remained for longer time, which may be related to the complex etiology of PACNS and the low response to clinical treatment.6 In comparison, in the secondary CNSV group, most of the vascular walls showed significant qualitative and quantitative changes after 6 months treatment, which related to the control of inflammation and the reduction of the affected area.Conclusion
In conclusion, high-resolution magnetic resonance vascular wall imaging, i.e., CUBE MRI, has been demonstrated for the feasibility in assessing the treatment effect of PACNS and secondary CNSV. Therefore, CUBE MRI can be considered an effective tool in the evaluation of PACNS and secondary CNSV.Acknowledgements
References
1. Hajj-Ali RA, Calabrese LH. Diagnosis and classification of central nervous system vasculitis [J]. J Autoimmun,2014, 48 / 49: 149 / 152.
2. Jennette JC, Falk RJ, Bacon PA, Basu N, Cid M.C, Ferrario F, et al. 2012 Revised international Chapel Hill consensus conference nomenclature of vasculitides. Arthritis Rheum 2013;65:1-11.
3. Mandell D M,Mossabasha M,Qiao Y,et al.Intracranial Vessel Wall MRI:Principles and Expert Consensus Recommendations of the American Society of Neuroradiology[J].Ajnr Am J Neuroradiol,2017,38(2):218-229.
4. Mossa-Basha M, Shibata D K, Hallam D K, et al. Added Value of Vessel Wall Magnetic Resonance Imaging for Differentiation of Nonocclusive Intracranial Vasculopathies[J]. Stroke, 2017, 48(11):3026.
5. Obusez EC, Hui f, Hajj-Ali RA,et al. High-resolution MRI vessel wall imaging: spatial and temporal patterns of reversible cerebral vasoconstriction syndrome and central nervous system vasculitis[J]. AJNR,2014,35:1527-1532.
6. Salvarani C, Brown RD Jr, Christianson TJ, et al. Adult primary central nervous system vasculitis treatment and course: analysis of one hundred sixty-three patients. Arthritis Rheumatol 2015; 67: 1637-45.
Figures