1593
Association between Morphologies of Middle Cerebral Artery Occlusion on Vessel Wall Imaging and Cerebrovascular Events in Moyamoya Patients1Radiology, Xuanwu hospital, Capital Medical University, Beijing, China, 2Department of Neurosurgery, 307 Hospital of Chinese People's Liberation Army, Beijing, China, 3Biomedical Imaging Research Institute, Cedars Sinai Medical Center, Los Angeles, CA, United States, 4Radiology, Xuanwu Hospital, Capital Medical University, Beijing, China
Synopsis
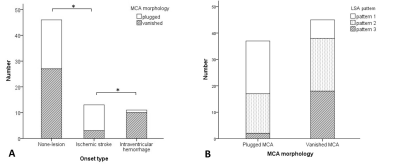
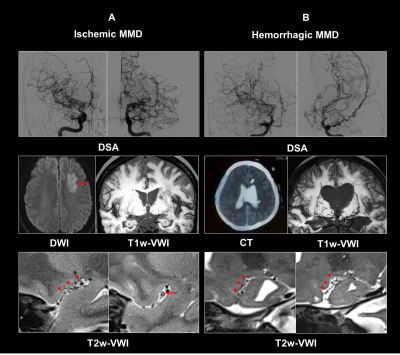
In this study, we used whole-brain vessel wall imaging (VWI) to characterize morphologies of middle cerebral artery (MCA) occlusion in patients with MMD, and explore their relationship to clinical findings. We found that plugged MCA was associated with ischemic stroke, however, vanishing MCA correlated with intraventricular hemorrhage. We also found that hemispheres with vanishing MCA manifested a higher degree of lenticulostriate artery (LSA) dilation and proliferation. The results suggest that there are two types of MCA occlusion in MMD, correlating with different stroke types and extent of perforator proliferation. Morphological analysis of occluded MCA using VWI may help understand the stroke mechanism of MMD.
Background and Purpose
Patients with moyamoya disease (MMD) can suffer from transient ischemic attack (TIA), ischemic stroke, or intracranial bleeding. However, the cause of ischemic attacks and intracranial hemorrhage is unclear. A recent study has suggested that morphological analysis of chronic middle cerebral artery (MCA) occlusion using vessel wall imaging (VWI) may help clarify the etiology of the disease 1. In clinical practice, we found that some MMD cases have a clear view of the occluded MCA trunk, but others just present with small dot-like MCA structures on VWI. Different morphologies of MCA occlusion may reflect distinct disease processes. Thus, we hypothesized that there are different morphological types of MCA occlusion in MMD, and morphologies of MCA occlusion are associated with clinical presentations and the extent of collateral vessels. Therefore, this study aimed to clarify the morphologies of MCA occlusion in patients with MMD, and explore their relationship to clinical findings using VWI, to help in elucidating the underlying mechanism of disease development.Material and methods
Patients with MMD were prospectively enrolled and underwent VWI exams. VWI was performed on a MAGNETOM Verio 3T MR system (Siemens Healthcare, Erlangen, Germany) with 3D T1-weighted and T2-weighted whole-brain vessel wall sequences: TR/TE = 900/15 ms (T1-weighted imaging) and 1800/177 ms (T2-weighted imaging); field of view = 170×170 mm2; 240 slices with slice thickness of 0.53 mm; voxel size = 0.53×0.53×0.53 mm3; and scan time = 8 min. Morphology of occluded MCA (plugged or vanishing) and the pattern of lenticulostriate artery (LSA) branches (pattern 1 = no dilation or proliferation, pattern 2 = mild dilation and proliferation, pattern 3 = dense dilation and proliferation) were evaluated for each hemisphere on VWI images. The included hemispheres in each MMD patient were individually classified as non-lesion, ischemic stroke, or intracranial hemorrhage (intraventricular hemorrhage, intraparenchymal hemorrhage, or subarachnoid hemorrhage). Odds ratios (ORs) of ischemic stroke (versus non-lesion subjects) and intraventricular hemorrhage (versus non-lesion subjects) with the respective 95% confidence intervals (CIs) were assessed using multivariable logistic regression, with MCA morphology as covariate, and adjusted by age, gender and Suzuki stage. Furthermore, ORs and corresponding 95% CIs for determining the association between LSA pattern and MCA morphology were calculated using multivariate logistic regression after adjusting for age and gender.Results
Forty-eight patients with 82 hemispheres with occluded MCA were enrolled. In total, 37 (45.1%) hemispheres exhibited plugged MCA and 45 (54.9%) manifested vanishing MCA. We found that hemispheres with vanishing MCA manifested a higher degree of LSA dilation and proliferation (pattern 2: adjusted odds ratio = 3.81, 95% confidence interval = 1.28-11.34, P = 0.016; pattern 3: adjusted odds ratio = 25.71, 95% confidence interval = 4.72-140.14, P < 0.001). To examine the relationship between MCA morphology and clinical presentation, 70 hemispheres were included and divided into 3 groups: hemispheres with non-lesion (n = 46), ischemic stroke (n = 13), and intraventricular hemorrhage (n = 11). Hemispheres without symptom (n = 22) or with TIA/headache (n = 24) were classified into non-lesion group. Multivariate logistic regression showed that plugged MCA was associated with ischemic stroke (adjusted odds ratio = 4.74, 95% confidence interval = 1.15-19.55, P = 0.031), however, vanishing MCA correlated with intraventricular hemorrhage (adjusted odds ratio = 10.93; 95% confidence interval = 1.19-100.33, P = 0.034). (Figure 1 and 2)Discussion
Two different types (plugged and vanishing) of the chronic occluded MCA on VWI has been previously reported, which suggests that the gross pathology of the occlusion might be different between two types 1. So the two different types of occluded MCA in MMD may suggest the different natural courses. A potential cause of plugged MCA in MMD is thickening of the fibrocellular intima and organization of the intraluminal thrombus. Scavenging activity decline of emboli is an important mechanism of brain infarction in patients with cerebral hypoperfusion. Our study gives the first description of thromboembolism (plugged type) via the VWI, and we prove that two types of MCA occlusion both exist in MMD by the radiological imaging view. We also found that plugged MCA was associated with ischemic stroke. This may be explained by assuming that thromboembolism mechanism causes ischemic stroke in patients with plugged MCA. We also found a significant relationship between vanishing MCA and intraventricular hemorrhage. The possible cause of vanishing MCA is the media shrinkage in MMD 2,3. A lower remodeling index in MMD compared to that of intracranial atherosclerotic disease is also reported in the literature 4,5. In patients with vanishing MCA, vessel hyperplasia develops in response to the chronic, progressive steno-occlusive changes in the MCA to compensate for reduced perfusion in the corresponding vascular territories, which may easily develop hemorrhagic events rather than ischemic stroke.Conclusion
In conclusion, both plugged and vanishing MCA are detected in patients with MMD. Vanishing MCA in MMD is associated with intraventricular hemorrhage, and abnormal dilation & proliferation of LSA branches. Plugged MCA in MMD correlates with ischemic stroke. This study suggests that morphological analysis of occluded MCA using VWI may help understand the pathophysiology of MMD, and potentially make different treatment strategies.Acknowledgements
We thank Dr. Cong Han and Zhiwen Liu from 307 Hospital of Chinese People's Liberation Army for their work in this study.
References
1. Kim S M, Ryu C W, Jahng G H, et al. Two Different Morphologies of Chronic Unilateral Middle Cerebral Artery Occlusion: Evaluation using High-Resolution MRI. Journal of neuroimaging: official journal of the American Society of Neuroimaging, 2013, 24(5):460-6.
2. Takekawa Y, Umezawa T, Ueno Y, et al. Pathological and immunohistochemical findings of an autopsy case of adult moyamoya disease. Neuropathology, 2004, 24(3):236-42.
3. Achrol AS, Guzman R, Lee M, Steinberg GK. Pathophysiology and genetic factors in moyamoya disease. Neurosurg Focus, 2009, 26(4):E4. doi: 10.3171/2009.1.FOCUS08302.
4. Mossa-Basha M, de Havenon A, Becker KJ, et al. Added value of vessel wall magnetic resonance imaging in the differentiation of moyamoya vasculopathies in a non-asian cohort. Stroke. 2016, 47(7):1782-8.
5. Ryoo S, Cha J, Kim SJ, et al. High-resolution magnetic resonance wall imaging findings of moyamoya disease. Stroke, 2014, 45(8):2457-60.
Figures