1587
BOLD Responses to Breath-by-Breath O2-CO2 Exchange Ratio Under Breath Hold Challenge in Mild Traumatic Brain Injury Patients1Athinoula A. Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Boston, MA, United States, 2Neurology, Massachusetts General Hospital, Boston, MA, United States
Synopsis
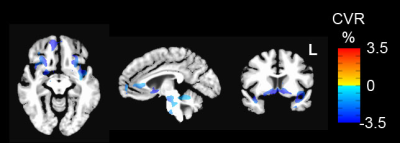
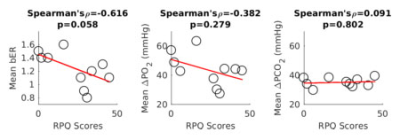
We used fMRI to map BOLD responses to breath-by-breath O2-CO2 exchange ratio (bER) under breath hold protocol for patients with persistent symptoms from mild traumatic brain injury (mTBI). Comparing to controls, reduced cerebrovascular reactivity (CVR) to bER was reported for patients in insula, anterior cingulate, nucleus accumbens and ventral tegmental area, basically regions which overlapped with the dopamine pathway. The mean resting bER decreased with increased symptom severity indicated by burden scores. Our findings are consistent with impaired dopamine pathway reported for TBI patients and show the success of using bER to evaluate CVR to breath hold.
Introduction
The brain of patients with mild traumatic brain injury (mTBI) can often appear normal on conventional clinical imaging including computed tomography (CT) and magnetic resonance imaging (MRI). There is still an unmet need of an imaging strategy with increased sensitivity to characterize the injury as well as the post-concussion symptoms (PCS) after the injury. Instead of using exogenous CO2 challenge which is often used to evaluate cerebrovascular reactivity (CVR) in patients, in this study, we used the changes of endogenous gases during breath holding to evaluate the cerebrovascular responses in patients with mTBI. Disturbances in respiratory functions after TBI are often accompanied by hypoxia1 which can lead to disturbances in brain gas exchange and disorders of the cerebral acid-base balance due to increased anaerobic metabolism.2, 3 Chronic hypoxemia and metabolic acidosis have been suggested to play an important role in the pathophysiological pathways that underlies the development of permanent brain damage. In a separate study on healthy subjects under breath hold challenge, our team has shown a strong dynamic coupling between cerebrovascular responses and breath-by-breath ratio of changes of partial pressures of O2 (PO2) to CO2 (PCO2), in short, breath-by-breath O2-CO2 exchange ratio (bER). In this study, we measured the blood oxygenation level dependent (BOLD) signal changes to bER in patients with mTBI under breath hold challenge. The successful application of bER in evaluating CVR under breath hold challenge would offer an alternative technique to exogenous CO2 challenge for patients with acute injuries.Subjects and Methods
Participants: A total of 21 subjects aged from 20 to 49 years were included in this study. Ten of them were patients with mild TBI (no loss of consciousness or loss of consciousness of <30 minutes’ duration, and the Glasgow Coma Scale (GCS) score was >=13). The remaining 11 subjects were healthy controls without brain injury. Methods: MRI scanning was performed on a 3-Tesla scanner (Siemens Medical Germany) in the Athinoula A. Martinos Center for Biomedical Imaging at the Massachusetts General Hospital. All the experimental procedures were explained to the subjects, and signed informed consent was obtained prior to participation in the study. Whole brain MRI datasets were acquired for each subject: 1) T1-weighted 3D-MEMPRAGE; 2) BOLD-fMRI images (TR=1450ms, TE=30ms, flip angle=90º, FOV=220×220mm, matrix=64×64, slice thickness=5mm, slice gap=1mm) acquired when the subject were under breath hold challenge. The paradigm consisted of 2 consecutive phases (resting and breath holding) repeated 6 times. The resting phase lasted no less than 60 seconds, while the breath holding phase lasted 30 seconds. The challenge lasted 10 minutes. Before MRI acquisition when the subjects were at rest and during MRI acquisition when the subjects were under breath hold challenge, physiological changes including PCO2, PO2 and respiration were measured by calibrated gas analyzers and respiratory bellow. Symptom burden was assessed using Rivermead Post Concussion Questionnaire (RPQ). Data analysis: During resting state and under breath hold challenge, time series of bER were derived as the ratio of the change in PO2 (ΔPO2 = inspired PO2 – expired PO2) to the change in PCO2 (ΔPCO2 = expired PCO2 – inspired PCO2) measured between end inspiration and end expiration in each respiratory cycle. All the BOLD-fMRI data were imported into the software AFNI4 for time-shift correction, motion correction, normalization and detrending. CVR in each voxel was derived by regressing ΔBOLD on bER acquired under breath hold challenge. Individual subject maps of CVR with ΔBOLD per unit change of bER were derived. Maps of ΔBOLD/bER from mTBI and control groups were compared using unpaired t-tests. All the statistical parametric maps will be cluster-corrected using a threshold estimated with Monte Carlo simulation algorithm. The time series of bER acquired during resting state was averaged to correlate with the RPQ scores.Results
Comparing with controls without brain injury, reduced CVR was observed in insula, anterior cingulate, nucleus accumbens, ventral tegmental area in patients with mTBI (Fig1). Most of the brain regions overlapped with the regions of dopamine pathway.5 The mean resting bER decreased with increased symptom severity indicated by RPQ scores (Fig2).Discussion
While the physiological mechanisms underlying the strong correlation between bER and ΔBOLD under breath hold challenge are not completely understood, our team found in another study on healthy subjects that bER and ΔPO2 are superior to ΔPCO2 to map the cerebrovascular responses to the brief breath hold challenge. Our finding of inverse relationship between resting bER and RPQ scores in 10 patients with mTBI is consistent with some extent of respiratory decline reported in previous studies.1-3 Reduced CVR found in the brain regions overlapping with those on the dopamine pathway in mTBI patients may explain the persistence of symptoms.Conclusion
Our fMRI findings are consistent with the impaired dopamine pathway reported in the literature on TBI patients. It also shows the success of using bER to evaluate CVR in patients with mTBI under breath hold challenge which has the potential to serve as an alternative approach to study CVR for patients with acute injuries.Acknowledgements
This research was carried out in whole at the Athinoula A. Martinos Center for Biomedical Imaging at the Massachusetts General Hospital, using resources provided by the Center for Functional Neuroimaging Technologies, P41EB015896, a P41 Biotechnology Resource Grant supported by the National Institute of Biomedical Imaging and Bioengineering (NIBIB), National Institutes of Health, as well as the Shared Instrumentation Grant S10RR023043.References
1. Sharma G, Goodwin J. Effect of aging on respiratory system physiology and immunology. Clin Interv Aging 2006;1:253-260.
2. Froman C. Alterations of respiratory function in patients with severe head injuries. Br J Anaesth 1968;40:354-360.
3. Zupping R. Cerebral acid-base and gas metabolism in brain injury. J Neurosurg 1970;33:498-505.
4. Cox RW. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Computers and Biomedical Research 1996;29:162-173.
5. Le Moal M, Simon H. Mesocorticolimbic dopaminergic network: functional and regulatory roles. Physiol Rev 1991;71:155-234.
Figures