1586
Yield of peri-ictal arterial spin-labelling MRI perfusion in refractory epilepsy1Nueroimaging and Interventional Radiology, National Institute of Mental Health and, Bangalore, India, 2Diagnostic and Interventional Radiology, All India Institute of Medical Sciences,, Jodhpur, India, 3Neurology, National Institute of Mental Health and, Bangalore, India
Synopsis
Arterial Spin Labelling (ASL), a non-invasive MR based perfusion technique, has emerged as an excellent method for quantifying brain perfusion and its potential in detecting perfusion changes in drug resistant epilepsy. Our study also demonstrates the perfusion changes in the epileptogenic zone with good concordance with structural MRI and video-EEG findings.
Methods: In this study, we included patients (n=29) with drug-resistant localization related epilepsy5 with positive video-EEG findings undergoing presurgical evaluation (Both temporal and neocortical causes of epilepsy). MRI: MRI were obtained on 3T Philips Achieva using 32-channel head-coil. sMRI and pCASL data were acquired immediate peri-ictal period. A High-resolution 3D-TFE T1W-images were acquired (TR/TE=8.2/3.7ms, Flip-angle=80, and spatial-resolution=1x1x1mm).
ASL-perfusion data was also acquired with following parameters: TR/TE=4400/14ms; dynamic-scans=40, slice-thickness=7mm, Post-label delay and labelling duration=1800sm; respectively. The video-EEG was also recorded using 10-20 channel EEG (Galileo NT, EB Neuro, Italy) machine.
PET: FDG-PET was acquired using a PET-MRI scanner (Biograph, Siemens; Erlangen, Germany). PET images were acquired in 3D-mode after intravenous injection of 5 MBq/kg of 18-fluor-FDG.
Data Analysis: Hyper-perfusion and hypo-perfusion pattern on ASL were designated based on visual analysis. Similarly, PET scans were analysed for the presence of hypo- or hyper-metabolism. To assess the concordance between ASL and other tests, the kappa coefficient was calculated. The degree of concordance was determined as follows:
(1) Discordant: Location of abnormality on ASL and the other test (e.g., video-EEG, sMRI, and PET-MR) was not matching or ASL was normal.
(2) Partially Concordant: CBF alteration on ASL was diffuse or larger as compared with any of the modality and localization overlapped partially.
(3) Concordant: Location of CBF abnormality on ASL was identical to those detected by other investigations at the sub-lobar level. Perfusion abnormalities in ASL determined after visual inspection were compared with conventional MRI findings, PET findings, and video-EEG data. The pathological area determined by the different methods were localized to various anatomical cortical regions in a blinded fashion.
Result: Of 29 patients [15M/14F; mean age=20.1±8years], 25 patients had lesions on structural MRI. ASL showed perfusion changes in 27 patients (hyper-perfusion=10, hypo-perfusion=17, and normal=2) with mean seizure to ASL scan duration of 6-hours (range 1-20hours). ASL had good concordance with structural MRI (20/29, 68.9% k= 0.638), and moderate concordance with video-EEG (k= 0.569).
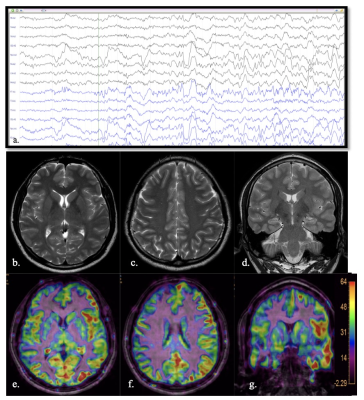
MRI Negative cases: All the four patients with normal MRI, labeled as cryptogenic, showed perfusion abnormalities on ASL (3 patients showed hyper-perfusion and 1 had hypo-perfusion). The final diagnosis in these cases were established by the consensus of the epilepsy team based on clinical history, neuropsychological assessment and electrophysiological findings from video-EEG monitoring. The perfusion abnormality in ASL was concordant with the final consensus diagnosis in all the four cases. Histopathological diagnosis was present in one case (Fig. 1), which revealed left parieto-occipital focal cortical dysplasia.
PET and ASL: FDG-PET data were available for 15 patients. It showed hypo-metabolism in 14 of these patients and was normal in one case. Complete concordance between ASL and FDG-PET was found in 10 patients, partial concordance in 2 patients, and 3 cases were non-concordant. One case where PET was studied as normal, showed hyper-perfusion in ASL imaging, with epileptogenic site correlating with the Video-EEG (k= 0.661).
Discussion: In this study peri-ictal ASL showed good concordance with the localization results obtained with clinical, electrophysiological and other imaging methods. In addition, ASL was able to show focal perfusion abnormalities in 4 patients who were otherwise negative on conventional MRI and electrophysiology correlated with the focus of abnormality shown by ASL in all the cases. The perfusion changes during the inter-ictal/-ictal/immediate post-ictal stage reflect changes in the neuronal activity. These events of perfusion changes occur typically over a period of minutes to several hours6. Thus, the perfusion changes in the epileptogenic zone are a dynamic phenomenon with a possible transformation from initial hyper-perfusion to hypo-perfusion during later stages. Hyper-perfusion is noted due to an elevation of the local cerebral metabolic rate for oxygen and glucose with a consequent increase in CBF in local tissue. Similarly; post-ictal hypo-perfusion is presumed to be the result of post-ictal exhaustion/ inhibition or a steal phenomenon associated with the propagation of -ictal discharges to adjacent brain areas.
Conclusion: This study indicates that ASL perfusion could be incorporated into the presurgical evaluation of all patients with localization-related epilepsy as it may reveal seizure-induced alteration in brain perfusion and may help to identify the location and extent of the epileptogenic zone.
Acknowledgements
No acknowledgement found.References
1. Jette N, Reid AY, Wiebe S. Surgical management of epilepsy. Canadian Medical Association Journal. 2014 Sep 16;186(13):997-1004.
2. Miller JW, Hakimian S. Surgical treatment of epilepsy. Continuum: Lifelong Learning in Neurology. 2013 Jun;19(3 Epilepsy):730.
3. Von Oertzen J, Urbach H, Jungbluth S, et al Standard magnetic resonance imaging is inadequate for patients with refractory focal epilepsy. Journal of Neurology, Neurosurgery & Psychiatry 2002;73:643-647. 4. Pittau F, Grouiller F, Spinelli L, Seeck M, Michel CM, Vulliemoz S. The role of functional neuroimaging in pre-surgical epilepsy evaluation. Frontiers in neurology. 2014 Mar 24;5:31.
5. Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Allen Hauser W, Mathern G, et al. Definition of drug resistant epilepsy: Consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic Strategies. Epilepsia. 2010 Jun 1;51(6):1069–77.
6. Duncan R. Ictal SPECT in Focal epilepsy. Epileptologie 2004; 21: 105 – 108.
Figures