1576
Gray Matter Changes of Pain-matrix Network in Patients with Acute Carbon Monoxide Intoxication1Department of Medical Imaging and Radiological Sciences, Kaohsiung Medical University, Kaohsiung, Taiwan, 2Department of Neurology, E-Da Hospital, Kaohsiung, Taiwan, 3Department of Radiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan
Synopsis
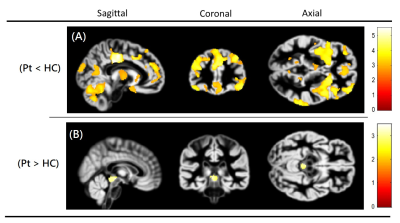
This study performed a voxel-based morphometry to investigate global gray matter changes in patients with acute CO intoxication. The results show significantly decreased gray matter volumes mostly in the pain-matrix regions, and significantly increased gray matter volumes in the periaqueductal gray (pain-modulating center). In the pain-matrix regions, the GM volumes were significantly negatively correlated with duration of coma, suggesting that longer duration of coma may lead to more headache symptoms in patients with acute CO intoxication.
Introduction
Carbon monoxide (CO) intoxication has been demonstrated to cause gray matter (GM) changes and headache symptom in CO patients. Headache is the most common neurological symptom in CO patients even with low exposure level, and the pathophysiology of headache might be characterized as an abnormality in the pain-modulating network1,2. A previous study demonstrated that voxel-based morphometry (VBM) is capable of detecting GM changes in the pain-matrix network of the brain in migraineurs3, but the headache-associated GM changes are not well understood. The purpose of this study was to perform a VBM analysis to investigate GM changes of the pain-matrix network in patients with acute CO intoxication.Methods:
This study was approved by the local institutional review board, and all subjects provided written informed consent before participating in this study. We enrolled 24 patients with acute CO intoxication (≤ 1 month) and 20 age- and gender- matched healthy controls. MRI was performed on a 1.5T MR scanner (Signa HDx, GE Healthcare, Milwaukee, Wisconsin) with an 8-channel phased-array head coil. Whole-brain T1-weighted imaging data were acquired from all participants and were post-processed using CAT12 (Computational Analysis Tool, run by SPM12) toolbox (http://www.neuro.uni-jena.de/cat/). In group comparisons, we performed a voxel-wise two-samples t-test to understand the GM differences between patient and control groups with age and gender as covariates. The difference was considered significant if cluster-level corrected P < 0.05 (uncorrected P<0.01 and cluster > 200 voxels). In addition, a non-parametric Spearman’s rank correlation coefficient was calculated to understand associations between GM volume and duration of coma in CO patients, and statistical significance was determined as P<0.05.Results and Discussion:
In acute CO patients, GM volumes were significantly decreased mainly in the frontal and occipital lobes, as well as in the central GM structures, as shown in Fig. 1A. These regions included cerebellum, amygdala, hypothalamus, thalamus, insula, anterior and posterior cingulate, prefrontal cortex, supplementary motor area, somatosensory cortex, secondary somatosensory cortex, and parietal cortex. However, the GM volumes were significantly increased in the periaqueductal gray (pain-modulating center) in CO patients, as shown in Fig. 1B. These findings suggest that GM changes are mostly in the pain-matrix network and are likely associated with headache symptoms in CO patients. In addition, the correlation analysis revealed that GM volumes were significantly negatively correlated with duration of coma in prefrontal cortex (r=-0.49), posterior cingulate cortex (r=-0.49), insula (r=-0.46) and amygdala (r=-0.50), suggesting that the duration of coma was associated with decrease of GM volume in the pain-matrix regions. Therefore, we concluded that VBM analysis is helpful to understand the headache-associated GM changes in patients with acute CO intoxication.Acknowledgements
No acknowledgement found.References
1. Weaver LK. Carbon Monoxide Poisoning. New England Journal of Medicine. 2009; 360: 1217-1225.
2. Arngrim N, Schytz HW, Hauge MK, Ashina M, Olesen J. Carbon monoxide may be an important molecule in migraine and other headaches. Cephalalgia. 2014; 34: 1169-1180.
3. Rocca MA, Ceccarelli A, Falini A, Colombo B, Tortorella P, et al. Brain gray matter changes in migraine patients with T2-visible lesions - A 3-T MRI study. Stroke. 2006; 37: 1765-1770.