1558
Increased Cerebral Blood flow was Correlated with Neurocognitive Dysfunction in Chronic Hemodialysis Patients: A Arterial Spin Labeling Study1Department of Radiology, Tianjin First Central Hospital, Tianjin Medical Imaging Institute, Tianjin, China, 2School of Graduates, Tianjin Medical Univeristy, Tianjin, China, 3Department of Hemodialysis, Tianjin First Central Hospital, Tianjin, China, 4MR Collaboration, Siemens Healthcare Ltd., Beijing, China
Synopsis
Cerebral blood flow (CBF) can be significantly reduced during a single hemodialysis session. However, few studies have investigated the effect of long-term hemodialysis on CBF and its correlation with neuropsychological tests. This study used pulsed arterial spin labeling to show that hemodialysis patients had significantly increased CBF in some cerebral regions. Increased CBF of the right opercular and triangular part of inferior frontal gyrus was negatively correlated with Mini Mental State Examination (MMSE) scores, and after adjusting for hemoglobin and hematocrit levels, these correlations became stronger. Dialysis duration, hemoglobin, hematocrit, and serum phosphorus were clinical risk factors for increased CBF.
Introduction
Neurocognitive impairment is an extremely common complication in hemodialysis patients, with as much as a 70% prevalence rate.1 The neuropathogenesis of neurocognitive impairment in hemodialysis patients remain poorly understood.2 Hemodialysis could theoretically affect cerebral macro- and microvascular blood flow changes because of the repetitive elimination of fluid, extracorporeal blood circulation, and other factors.3,4 Thus, recognizing cerebral blood flow (CBF) changes is important to understand the neurologic mechanisms that underly neurocognitive impairment. Few studies have investigated the long-term effects of hemodialysis on cerebral circulation, and the results have been inconsistent.5,6 Therefore, our study aimed to 1) investigate CBF changes in hemodialysis patients compared with age-, sex-, and education-matched healthy controls using pulsed arterial spin labeling (ASL); 2) investigate the correlations between CBF changes and neuropsychological test scores; and 3) investigate the clinical risk factors for CBF changes.Materials and methods
Thirty-two patients and 35 age-, gender-, and education-matched healthy controls (HCs) participated in this study. All subjects were right-handed and did not have any other health conditions; magnetic resonance imaging (MRI) contraindications were noted. Mini-Mental State Examinations (MMSE) were administered to evaluate neurocognitive function. MRI scans were performed on a 3 T MR scanner (MAGNETOM Trio a Tim System, Siemens Healthcare, Erlangen, Germany) and included routine ASL and T1-MPRAGE. The parameters of these two sequences were: ASL: field of view = 230×230mm2, flip angle = 90°, TR = 2300ms, TE = 12ms, TI1/TI2 = 700/1800ms, slices = 25, voxel size = 2.9×2.9×4.0mm3, and acquisition time = 268sec; T1-MPRAGE: field of view = 250×250mm2, flip angle = 9°, TR = 1900ms, TE = 2.52ms, TI = 900ms, slices = 176, voxel size = 1.0×1.0×1.0mm3, and acquisition time = 258sec. ASL images were preprocessed using a SPM8 (http://www.fil.ion.ucl.ac.uk/spm/)-based ASL Data Processing Toolbox (http://www.cfn.upenn.edu) to acquire the CBF parametric maps of hemodialysis patients and HCs.Two independent-samples t-test was used to compare the differences in CBF between patients and HCs (Bonferroni correction). Pearson correlation analysis was used to investigate the relationship between the neuropsychological tests and CBF changes in patients. Considering that anemia is a predominant risk factor for neurocognitive impairment, partial correlation analysis was further performed with hemoglobin and hematocrit as covariates. The multiple stepwise regression analysis was used to investigate the clinical risk factors for CBF changes in patients. P-values less than 0.05 were considered statistically significant.
Results
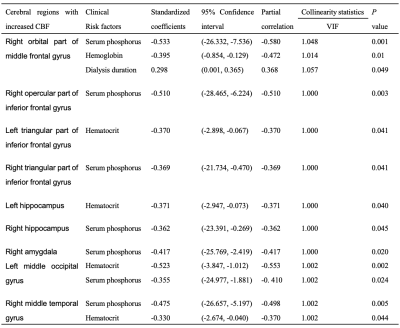
The clinical data of hemodialysis patients and HCs are presented in Fig. 1. The CBF of the right orbital region of the middle frontal gyrus, right opercular region of the inferior frontal gyrus, bilateral triangular region of the inferior frontal gyrus, bilateral hippocampus, right amygdala, left middle occipital gyrus, right putamen, and right middle temporal gyrus were significantly increased in patients compared with the HCs ( all P<0.001, Bonferroni correction) (Fig. 2). The largest peak intensity of each brain region between patients and HCs is shown in Fig. 3. The increased CBF of the right opercular and triangular regions of the inferior frontal gyrus was negatively correlated with MMSE scores (r=-0.502, P=0.004; r=-0.423, P=0.018) (Fig. 4). Because anemia is a predominant risk factor for neurocognitive impairment, the two correlations above became stronger after adjusting for hemoglobin and hematocrit levels (r=-0.516, P=0.005; r=-0.439, P=0.019) (Fig. 4). Dialysis duration, and hemoglobin, hematocrit, and serum phosphorus levels were independent predictive factors for increased CBF in hemodialysis patients (all P<0.05) (Fig. 5).Discussion
We found significantly increased CBF in several regions of the brain in hemodialysis patients compared with HCs. These regions are primarily responsible for speech, emotional processing, memory, cognitive processing, visual information, and motor execution. Increased CBF of the right opercular and triangular regions of the inferior frontal gyrus was negatively correlated with MMSE scores, and after adjusting for hemoglobin and hematocrit levels, these correlations became stronger. These findings indicated that both anemia and increased CBF in these areas were responsible for the neurocognitive impairment. It has been reported that increased CBF was supposed as the some form of compensatory mechanism (e.g. neural activity) during the early stage of clinical syndrome, especially during the mild cognitive impairment,7 and dialysis duration, hemoglobin, hematocrit, and serum phosphorus levels were independent predictive factors for increased CBF in hemodialysis patients.Conclusions
Chronic hemodialysis can cause increased CBF, which was found to be negatively correlated with neurocognitive impairment, and the correlations became even stronger after adjusting for the effect of anemia. Dialysis duration, hemoglobin, hematocrit, and serum phosphorus levels were found to be clinical risk factors for increased CBF.Acknowledgements
This work was supported by the Natural Scientific Foundation of China (grant number 81901728 to Chao Chai, grant number 81871342 to Shuang Xia).References
1. Murray AM, Tupper DE, Knopman DS, Gilbertson DT, Pederson SL, Li S, et al.: Cognitive impairment in hemodialysis patients is common. Neurology 67: 216–223, 2006; 3
2. Wierenga CE, Dev SI, Shin DD, et al. Effect of mild cognitive impairment and APOE genotype on resting cerebral blood flow and its association with cognition. J Cereb Blood Flow Metab 2012; 32(8): 1589-9159.
3. Polinder-Bos HA, García DV, Kuipers J, Elting JWJ, Aries MJH, Krijnen WP, Et al. Hemodialysis Induces an Acute Decline in Cerebral Blood Flow in Elderly Patients. J Am Soc Nephrol. 2018 Apr;29(4):1317-1325.
4. Findlay MD, Dawson J, Dickie DA, Forbes KP, McGlynn D, Quinn T, et al. Investigating the Relationship between Cerebral Blood Flow and Cognitive Function in Hemodialysis Patients. J Am Soc Nephrol. 2019 Jan;30(1):147-158.
5. Prohovnik I, Post J, Uribarri J, Lee H, Sandu O, Langhoff E. Cerebrovascular effects of hemodialysis in chronic kidney disease. J Cereb Blood Flow Metab. 2007 Nov;27(11):1861-9.
6. Jiang XL, Wen JQ, Zhang LJ, Zheng G, Li X, Zhang Z, Liu Y, Zheng LJ, Wu L, Chen HJ, Kong X, Luo S, Lu GM, Ji XM, Zhang ZJ. Cerebral blood flow changes in hemodialysis and peritoneal dialysis patients: an arterial-spin labeling MR imaging. Metab Brain Dis. 2016 Aug;31(4):929-36.
7. Dai W, Lopez OL, Carmichael OT, Becker JT, Kuller LH, Gach HM. Mild cognitive impairment and alzheimer disease: patterns of altered cerebral blood flow at MR imaging. Radiology. 2009 Mar;250(3):856-66.
Figures
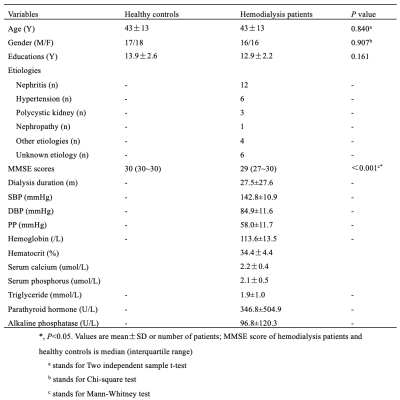
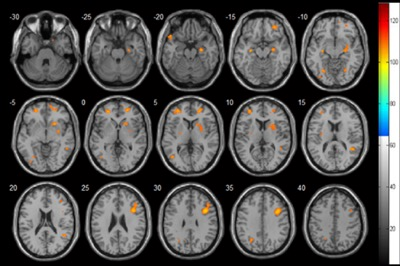
Fig. 2 The brain areas that showed significant cerebral blood flow differences between hemodialysis patients and healthy controls.
CBF was increased in the right orbital part of the middle frontal gyrus, right opercular part of the inferior frontal gyrus, bilateral triangular part of the inferior frontal gyrus, bilateral hippocampus, right amygdala, left middle occipital gyrus, right putamen, and right middle temporal gyrus in hemodialysis patients compared with healthy controls (P<0.001, Bonferroni corrected).
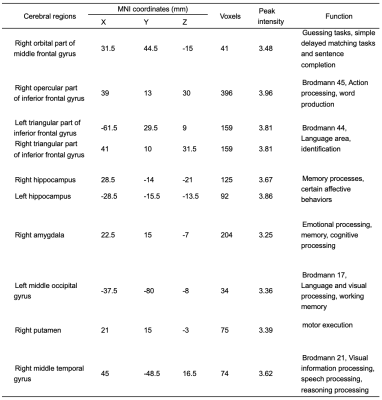
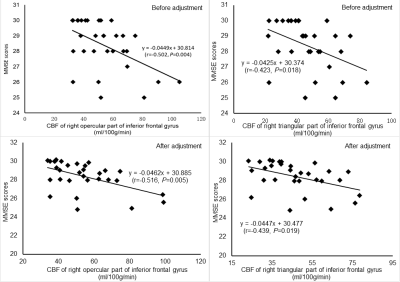
Fig. 4 Correlations between cerebral blood flow (CBF) and mini-mental state examination(MMSE) scores in hemodialysis patients.
Increased CBF of the right opercular and triangular part of the inferior frontal gyrus was negatively correlated with MMSE scores (r=-0.502, P=0.004; r=-0.423, P=0.018). Considering that the anemia was a predominant risk factor for neurocognitive impairment, the above two correlations became stronger after adjusting for hemoglobin and hematocrit levels (r=-0.516, P=0.005; r=-0.439, P=0.019).