1496
Different patterns of perfusion changes in tremor-dominant Parkinson’s disease and essential tremor using 3D arterial spin labeling imaging1GE Healthcare, Shanghai, China, 2Zhongshan Hospital, Shanghai, China, 3GE Healthcare, Beijing, China
Synopsis
This preliminary study aimed to identify potential markers in diagnosis of tremor disorders such as tremor-dominant Parkinson’s disease (PDT) and essential tremor (ET). A novel 3D pulsed-continuous arterial spin labeling technique (3D pCASL) was used to provide whole brain quantitative perfusion measurement, followed by voxel-wise comparison to evaluate regional CBF characteristics in patients with PDT, ET and age- and gender- matched healthy controls. PDT patients showed decreased CBF in the caudate and precuneus when compared to ET patients. The altered metabolic patterns of PDT and ET can help to understand different pathophysiological mechanism of tremor disorders.
Purpose
Essential tremor (ET) is the most common motor disorder in the elderly, while the etiology and pathophysiology still have been a mystery. It remains a challenge to differentiate ET from tremor-dominant Parkinson’s disease (PDT) in the early stage. In recent years, arterial spin labeling (ASL) has been widely used in neurological and psychiatric disorders since arterial blood water can be used as an endogenous tracer for cerebral blood flow (CBF) measurement rather than radioactive tracer or other contrast agents, which is convenient for the clinical use.1 In this preliminary study, a novel 3D pulsed-continuous arterial spin labeling technique (3D pCASL) was used to provide whole brain quantitative perfusion measurement,2 followed by voxel-wise comparison to evaluate regional CBF characteristics in patients with PDT, ET and age- and gender- matched healthy controls. We aimed to identify potential markers in diagnosis of tremor disorders.Methods
All the subjects gave written informed consent to participate the study, which was approved by the local ethical committee. Twenty-four patients with untreated ET (aged 60.0±12.1 years, 12 females), 25 patients with de novo PDT (aged 62.8±7.7 years, 16 females) to eliminate the undefined confounding factors from medication, and 39 healthy control subjects (aged 61.9±6.7 years, 22 females) were recruited. ET patients were diagnosed according to the criteria of the Consensus Statement of the Movement Disorders Society on Tremor. PDT patients were diagnosed according to the criteria of the MDS clinical diagnostic criteria for Parkinson's disease. All the patients were drug naive. Perfusion scans were performed with a 3.0-T MR750 scanner (GE Healthcare, Milwaukee, WI) using an 8-channel phase array head coil. Two sets of ASL images were acquired with and without the spatially selective inversion (tagging) pulse (TR/TE 4830/10 ms, flip angle 155°, labeling duration 1.5 s, post label delay 1.5 s, matrix =128x128, FOV 24 cm, thickness/gap 4/0 mm). The difference maps between the tag and control pairs were averaged for each subject and quantitative cerebral blood flow (CBF) maps were calculated with the vender provided toolbox. Image pre-processing was performed using SPM8 (http://www.fil.ion.ucl.ac.uk/spm). Spatial transformation included a three-dimensional rigid body registration to correct for head motion, followed by a nonlinear warping to spatially normalized CBF maps into a standard stereotaxic space. The normalized CBF maps were resampled to 2x2x2 mm3 isotropic voxel size and smoothed with a 6 mm isotropic Gaussian kernel. Voxel-based analyses was conducted using one-way ANOVA to make comparison among ET, PDT and control groups. The post-hoc two-sample T test was used to compare the differences between each two groups. The AlphaSim program implemented in AFNI (http://afni.nimh.nih.gov/pub/dist/doc/manual/AlphaSim.pdf) was used for multiple comparison correction (corrected p<0.05).Results
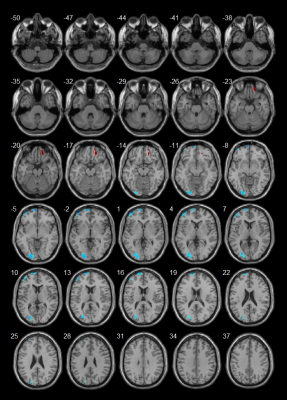
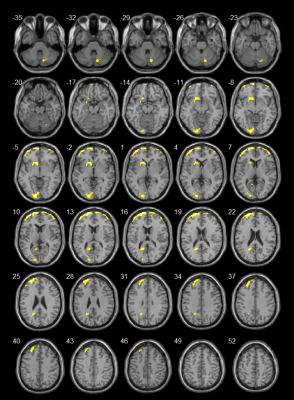
PDT patients showed decreased CBF in left superior and middle frontal gyrus, and left lingual gyrus as compared to healthy controls, while increased CBF in the right superior frontal gyrus (Fig 1). No significant CBF differences were found between ET patients and healthy controls. More interestingly, for the comparison between PDT and ET patients, the PDT patients showed hypoperfusion regions in the right cerebellum posterior lobe, left caudate, bilateral superior and middle frontal gyrus, left lingual gyrus and precuneus (Fig 2).Discussion and Conclusion
PDT patients exhibited consistent CBF decrease in left superior and middle frontal gyrus, and left lingual gyrus as compared to ET patients and healthy controls. Furthermore, PDT patients showed CBF deficits in the caudate and precuneus when compared to ET patients. The caudate nucleus has long been associated with motor processes due to its role in Parkinson's disease and the precuneus has been suggested to be involved in directing attention in space. The altered metabolic patterns of ET and PDT can help to understand different pathophysiological mechanism of tremor disorders. ASL perfusion may be used as a sensitive marker for diagnosis and evaluation of disease progression.Acknowledgements
No acknowledgement found.References
1. Ding B, Lin H, Zhang Y, et al. Pattern of cerebral hyperperfusion in Alzheimer’s disease and amnestic mild cognitive impairment using voxel-based analysis of 3D arterial spin-labeling imaging: initial experience. Clinical Interventions in Aging. 2014;9:493–500.
2. Dai W, Garcia D, de Bazelaire C, et al. Continuous flow-driven inversion for arterial spin labeling using pulsed radio frequency and gradient fields. Magn Reson Med. 2008;60(6):1488-1497.