1400
"Comparative analysis of 3D DIR and 3D FLAIR in cases of acute optic neuritis"1Neuroimaging and interventional radiology, national institute of mental health and neuroscineces (NIMHANS) bangalore, india, Bangalore, India, Bangalore, India, 2Neurology, national institute of mental health and neuroscineces (NIMHANS) bangalore, india, Bangalore, India, Bangalore, India, 3Neuroanaesthesia, national institute of mental health and neuroscineces (NIMHANS) bangalore, india, Bangalore, India, Bangalore, India, 4radiology, Fortis Hospital, Gurugram, India
Synopsis
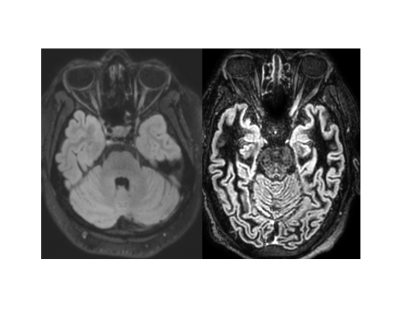
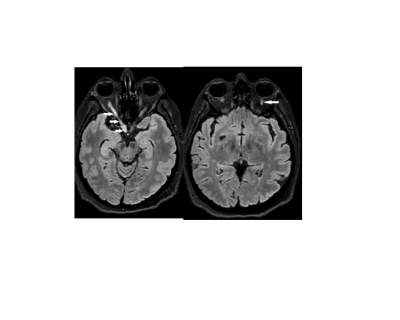
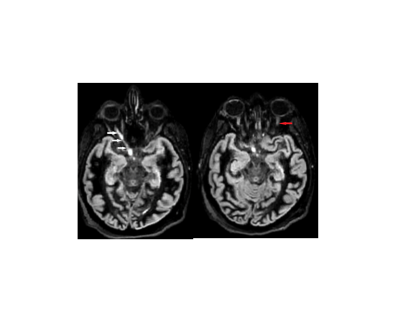
Optic neuritis is presenting feature in 15-20% cases of MS and 50% cases of MS have optic neuritis during course of illness. Signals from CSF and intraorbital fat are main hurdles in optic nerve imaging, 3D FLAIR and 3D DIR are used to study optic nerve pathologies as they suppress fat and CSF signals. DIR nulls signal from NAWM providing inherent contrast. 3D DIR and 3D FLAIR was done in 31 case of acute optic neuritis and 30 controls. We found higher contrast rates, sensitivity and negative predictive value for the 3D DIR than 3D FLAIR in acute optic neuritis
Introduction
Optic neuritis is inflammation of optic nerve with varied etiologies which includes demyelinating diseases, connective tissue disorder, infectious and parainfectious processes(1)(2). Optic neuritis is a clinical diagnosis and is aided by visual evoked potential (VEP). Due to presence of orbital fat and perioptic cerebrospinal fluid (CSF), for optic nerve imaging, T2-weighted sequences with both fat and water suppression are required. DIR (Double Inversion Recovery) involves two inversion pulses which suppress fluid and normal-appearing white matter(NAWM) which improves detection of lesions(3).Methods
This the study consist of 31 patients with acute optic neuritis confirmed by VEP, and 30 age and sex-matched controls. Imaging was performed on Philips 3T (Ingenia) scanner. MRI protocol consists of 3D FLAIR (Fluid Attenuated Inversion Recovery) and 3D DIR covering orbits and brain. SPIR (Selective Partial Inversion Recovery) was fat suppression method used. To reduce scanning time, compressed sensing was used. The optic nerve was divided into four segments intraorbital, intracanalicular, prechiasmatic and chiasm for localisation of signal abnormality. Each set of MR images (3D FLAIR, 3 D DIR reformats and multiplanar) was examined independently and separately by two observers for the detection of signal abnormality. Contrast rate (CR) [Signal intensity (SI) pathological segment-SI contralateral/SI contralateral x100] was calculated in unilateral cases optic neuritis (7). Mcnemars chi-square test was used to compare 3D FLAIR and 3 DIR in diagnosis of ON.Results
1) Intraobserver agreement kappa (K) values for 3D DIR for intraorbital, intracanalicular, prechiasmatic and optic chiasm were 1, 0.88, 0.87, and 0.91 respectively. Kappa values for intraorbital, intracanalicular, prechiasmatic and optic chiasm for 3 D FLAIR were 0.89, 0.85, 0.76 and 1 respectively.2) Interobserver agreement for 3D FLAIR kappa values for intraorbital, intracanalicular, prechiasmatic, and optic chiasm were 0.84, 0.83, 0.74 and 0.92 respectively. For 3D DIR kappa values for intraorbital, intracanalicular, prechiasmatic, and optic chiasm were 0.96, 0.83, 0.75 and 0.88 respectively.
3) Sensitivity for 3D FLAIR was 0.88, while Sensitivity for 3D DIR was 0.94. Negative predictive value(NPV) for 3D FLAIR was 0.88, while for 3D DIR it is 0.97.
4) Mean CR for 3D DIR was 109+/-45 while for 3D FLAIR 37+/-21 with P-value <0.001.
5) Mcnemars Chi-square test showed P-value of which was 0.371 which is not significant statistically, hence there is no significant difference in 3D FLAIR and DIR in diagnosing acute optic neuritis.
Discussion
In this study, 3D DIR and 3D FLAIR were performed in case and control population. The average age was 33.65 years and is consistent with literature(4)(5). Female: male ratio was 2.44 which is consistent with previously published studies(6). In terms, intraobserver and interobserver agreement for optic chiasm 3D FLAIR showed better performance. Since SPIR was used as fat suppression technique for DIR, loss of fat suppression was observed at air and bone interface which could offer a possible explanation for this observation. For intraorbital, prechiasmatic segments 3D DIR had a better intraobserver and interobserver correlation. Sensitivity and NPV for ON are better for 3D DIR. CR is higher for DIR than 3D FLAIR with P-value <0.001. A possible explanation for this is inherent contrast obtained due to suppression of CSF and NAWM in DIR(7)(8). We did not find any statistically significant difference in 3D FLAIR and 3D DIR in terms of diagnosis of optic neuritis (P-value 0.345) which is likely due to a smaller cohort. However, we found 2 cases in which 3D FLAIR failed to detect any abnormality while 3D DIR revealed signal changes. Limitation of our study includes VEP was not performed in control group population however, in unilateral optic neuritis cases contralateral radiologically normal nerve served as internal control. Children less than 12 years of age were excluded from study, because of less prevalence of optic neuritis in this cohort and co-operation for imaging is an issue in the paediatric age group. Time the interval between onset of symptoms and imaging was variable though it was within 14 days of onset of symptoms, also time interval between onset of symptoms and performance of VEP was variable. In future standardisation of the time interval between onset of symptoms and imaging and between imaging and VEP can be done. Also further studies including a larger cohort to compare 3D FLAIR and 3D DIR can be performed.Conclusion
3D DIR has CR, higher sensitivity and NPV than 3D FLAIR in diagnosing optic neuritis. Higher CR of DIR allow novice reader to diagnose optic neuritis with confidence. For diagnosing acute optic neuritis 3D FLAIR and 3D DIR did not found to have a not statistically significant difference. In future 3D FLAIR can be replaced with 3D DIR for evaluating acute optic neuritis.Acknowledgements
I acknowledge Dr Jitender Saini, Dr R.K. Gupta for the innovative idea of doing 3D DIR in acute optic neuritis. Their extremely sharp mind and intellectual assistance were key to completing the study. I also wanted to say thank you for Dr Nethravati M for diagnosing cases of acute optic neuritis and immediately referring for MRI and VEP. Diagnosing cases with acute optic neuritis was a key component of the study and it would not have been possible without her support Dr Dhritiman Chakraborty has helped me in all complicated statistical work. My sincere thanks to all the technologists, radiography students and staff of our department for their support in performing this study lastly, I would dedicate this work to my parents who raised me and made me the person I am today. I would also dedicate this to my late grandparents for their blessings and their immense love. They are my guardian angels who are always looking out for meI would like to say thanks to all patients who were recruited for the study,I sincerely hope that this work can be of some use to the patients in the future.References
1.Osborne B, Balcer LJ, Gonzalez-scarano F. Optic neuritis : Pathophysiology , clinical features , and diagnosis Optic neuritis : Pathophysiology , clinical features , and diagnosis. 2014;1–17.
2.Hoorbakht H. Optic Neuritis, its Differential Diagnosis and Management. Open Ophthalmol J. 2012;6(1):65–72.
3.Saranathan M, Worters PW, Rettmann DW, Winegar B, Becker J. Physics for clinicians: Fluid-attenuated inversion recovery (FLAIR) and double inversion recovery (DIR) Imaging. J Magn Reson Imaging. 2017;46(6):1590–600.
4.Jackson A, Sheppard S, Laitt RD, Kassner A, Moriarty D. Optic neuritis: MR imaging with combined fat- and water-suppression techniques. Radiology. 1998;206(1):57–63.
5.Helmut W, Martin S. Diagnostik und Therapie der Optikusneuritis. Dtsch Arztebl Int. 2015;112(37):616–26.
6.Famiglio LM. Optic neuritis. Treat Pediatr Neurol Disord. 2005;5(3):453–6.
7.Hodel J, Outteryck O, Bocher AL, Zéphir H, Lambert O, Benadjaoud MA, et al. Comparison of 3D double inversion recovery and 2D STIR FLAIR MR sequences for the imaging of optic neuritis: pilot study. Eur Radiol. 2014;24(12):3069–75.
8.Sartoretti T, Sartoretti E, Rauch S, Binkert C, Wyss M, Czell D, et al. How common is signal-intensity increase in optic nerve segments on 3D double inversion recovery sequences in visually asymptomatic patients with multiple sclerosis? Am J Neuroradiol. 2017;38(9):1748–53.
Figures