1398
Longitudinal progression of cortical thinning differs across MS phenotypes and is clinically relevant: a multicentre study
Paola Valsasina1, Maria A. Rocca1,2, Milagros Hidalgo de la Cruz1, Claudio Gobbi3, Antonio Gallo4, Chiara Zecca3, Alvino Bisecco4, and Massimo Filippi1,2,5
1Neuroimaging Research Unit, Institute of Experimental Neurology, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy, 2Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy, 3Department of Neurology, Neurocenter of Southern Switzerland, Civic Hospital, Lugano, Switzerland, 4Department of Advanced Medical and Surgical Sciences, and 3T MRI Center, University of Campania “Luigi Vanvitelli”, Naples, Italy, 5Vita-Salute San Raffaele University, Milan, Italy
1Neuroimaging Research Unit, Institute of Experimental Neurology, Division of Neuroscience, IRCCS San Raffaele Scientific Institute, Milan, Italy, 2Neurology Unit, IRCCS San Raffaele Scientific Institute, Milan, Italy, 3Department of Neurology, Neurocenter of Southern Switzerland, Civic Hospital, Lugano, Switzerland, 4Department of Advanced Medical and Surgical Sciences, and 3T MRI Center, University of Campania “Luigi Vanvitelli”, Naples, Italy, 5Vita-Salute San Raffaele University, Milan, Italy
Synopsis
In this study, we used cortical thickness analysis to investigate the evolution over time of cortical grey matter atrophy in a multicenter cohort of patients with multiple sclerosis (MS) acquired at 3 European sites. We detected a different susceptibility to cortical damage across the different clinical phenotypes of MS, with the involvement of temporal, parietal and occipital regions in relapsing-remitting MS, and an additional frontal involvement in progressive MS. Different annualized cortical thinning rates were found across MS clinical phenotypes. Cortical thinning in frontal and temporal areas was crucial for identifying patients with more severe disability at follow-up.
Introduction
Although multiple sclerosis (MS) was traditionally considered a white matter disease, the presence of widespread grey matter pathology (in particular, the atrophy of the cerebral cortex) has been recently demonstrated from the earliest stages of the disease [1]. Cortical thickness (CTh) is a sensitive measure of cortical pathology [2], contributing to explain a variety of clinical symptoms. Longitudinal investigations of cortical thinning in MS are still scanty. Aim of this study was to investigate the distribution and regional evolution of CTh reduction in patients with different MS clinical phenotypes in a multicentre dataset.Methods
Prospectively, T2- and 3D T1-weigthed images were acquired at 3.0 T from 86 MS patients (75 relapsing-remitting MS [RRMS], 11 progressive MS [PMS]) and 34 healthy controls (HC) at 3 European sites. Neurological assessment and MRI were performed at baseline and after one-year. Patients were classified as clinically stable or worsened according to their EDSS change [3]. Baseline CTh differences and changes over time were assessed on 3D T1-weighted images using the longitudinal stream of Freesurfer [4] in the whole MS group, in the main MS clinical phenotypes as well as in patients with and without disability progression.Results
At baseline, temporal and occipital atrophy was found in MS patients vs HC. RRMS patients mainly showed CTh loss in bilateral superior temporal and occipital regions vs HC (Figure 1), while PMS patients showed additional CTh reduction vs RRMS, mostly in inferior frontal regions (Figure 1). During the follow-up, MS patients showed significant within-group cortical thinning mainly in frontal, parietal and temporal areas (Figure 2), whereas no CTh changes were observed in HC. RRMS patients showed significant within-group cortical thinning over time mainly in superior frontal, parietal and occipital cortices (p<0.01 vs HC, Figure 2). In PMS patients, cortical thinning mainly involved the inferior frontal and temporal pole cortices, with a significant time-by-group interaction vs RRMS in these latter regions (Figure 2). Finally, cortical thinning was higher in frontal and temporal regions in clinically worsened (n=8) vs stable MS patients (Figure 3).Discussion
The pattern of cortical atrophy highlighted a different regional susceptibility to MS-related neurodegenerative processes throughout the different phases of the disease. This allowed us to identify brain areas in which neuroprotection programs may be targeted: temporal and occipital areas in relapsing-remitting MS patients, and an additional focus in inferior frontal regions in progressive MS patients. Cortical thinning over time in such cortical areas was correlated with higher clinical disability at follow-up.Conclusions
One-year cortical thinning progression was variable across MS phenotypes and contributed to explain clinical worsening.Acknowledgements
No acknowledgement found.References
[1] Filippi M., et al. Curr Opin Neurol, 2014. 27: 290-299. [2] Fischl B. et al. PNAS, 2000; 97: 11050-5. [3] Filippi, M., et al. Neurology, 2013. 81: 1759-1767. [4] Reuter M, et al. NeuroImage, 2012; 61: 1402-18.Figures
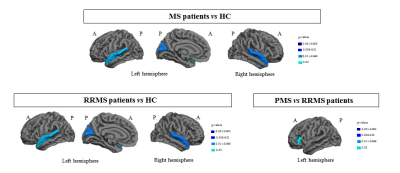
Figure 1.
Regions showing differences of cortical thickness between multiple sclerosis
(MS) patients and healthy controls (HC), between relapsing-remitting (RR) MS
patients and HC, and between RRMS and progressive (P) MS.
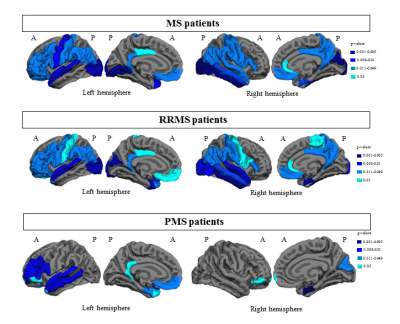
Figure 2. Regions showing
cortical thinning over time in multiple sclerosis (MS) patients, in
relapsing-remitting (RR) MS patients and in progressive (P) MS.
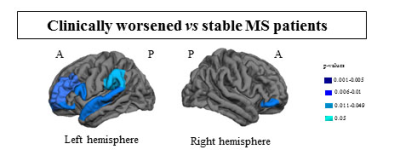
Figure 3.
Regions showing higher cortical thinning over time in clinically worsened vs stable multiple sclerosis (MS)
patients.