1337
Myocardial and Intraventricular Kinetic Energy in Patients with Repaired Tetralogy of Fallot
Shi-Ying Ke1, Meng-Chu Chang1, Ming-Ting Wu2, Ken-Pen Weng3,4, and Hsu-Hsia Peng1
1Department of Biomedical Engineering and Environmental Sciences, National TsingHua University, Hsinchu, Taiwan, 2Department of Radiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, 3Department of Pediatrics, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, 4Department of Pediatrics, National Yang-Ming University, Taipei, Taiwan
1Department of Biomedical Engineering and Environmental Sciences, National TsingHua University, Hsinchu, Taiwan, 2Department of Radiology, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, 3Department of Pediatrics, Kaohsiung Veterans General Hospital, Kaohsiung, Taiwan, 4Department of Pediatrics, National Yang-Ming University, Taipei, Taiwan
Synopsis
We aimed to investigate the interaction between myocardial kinetic energy (KEmyo) and intraventricular KE (KEven) in left- and right-ventricle (LV, RV) for repaired tetralogy of Fallot (rTOF) patients. The rTOF group displayed higher systolic RV KEven, earlier LV myocardial diastolic time-to-peak (TTPmyo), earlier RV TTPmyo in both systole and diastole, earlier LV TTPven in both systole and diastole, and earlier RV TTPven in systole. In conclusion, from an insight of energy conversion, rTOF patients demonstrated undermined interaction between LV KEmyo and KEven in an early stage. The dilated RV potentially have impacts on the RV KEven in rTOF patients.
Introduction
Patients with repaired tetralogy of Fallot (rTOF) is the most common form of cyanotic congenital heart.1 The kinetic energy (KE) is a measure of the amount of work involved directly in moving blood.2 The disturbed intraventricular KE in left and right ventricles (LV, RV) in rTOF patients was studied using 4D flow MRI.3,4 Previous study verified that altered RV hemodynamics interacted with severe pulmonary regurgitation (PR).5 Moreover, the association of RV myocardium adapted to pressure overload of rTOF patients was reported.6 Although these studies mentioned the myocardial and intraventricular KE, the potential impact of the myocardial KE on intraventricular flow KE has not been discussed thoroughly. In this study, we aimed to investigate the interaction between myocardial and intraventricular KE in both LV and RV for rTOF patients in an early stage with preserved cardiac function.Method
The study population comprised 48 rTOF patients (22.2±4.0 y/o; male/female: 29/19) and 46 age-matched normal volunteers (21.7±1.2 y/o; male/female: 28/18). Images were acquired at a 3-T clinical MR scanner (Tim Trio or Skyra, Siemens, Erlangen, Germany) with prospective ECG triggering and navigator-echo to synchronize with cardiac and respiratory motion, respectively. All subjects were imaged using 2D dark-blood fast low-angle shot sequence for tissue phase mapping (TPM) acquisitions. The protocol parameters were as follows: TR/TE = 6.5/4.2 ms, pixel size = 1.17 x 1.17 mm2, slice thickness = 6 mm, flip angle = 7°, acceleration factor = 5,Venc=15 and 25 cm/s for in-plane and through-plane motions, respectively, and temporal resolution=26 ms. The 4D flow dataset was acquired by TR/TE=10.8/2.9 ms, voxel size=3.2x1.4x3.5 mm3, flip angle=7°, Venc=150 cm/s, and temporal resolution=41.6 ms.A self-developed program was employed to calculate the longitudinal (vz), radial (vr), and circumferential (vØ) velocities in LV and RV and the corresponding myocardial KE (KEmyo).
The voxel-wise KEmyo was calculated as: $$KE_{myo}=\frac{1}{2}×ρ_{myo}×V_{myo}×v_{myo}^2 (1)$$where ρmyo was myocardial density with a value of 1050 kg/m3, Vmyo denoted voxel volume, and vmyo represented the voxel velocity. In the current work, we added upthree-directional components of KE as total KE.
As shown in Figure 1, the ROIs of LV and RV were manually determined in a 4-chamber view for calculation of intraventricular KE as follows:$$KE_{ven}=\frac{1}{2}×ρ_{ven}×V_{ven}×v_{ven}^2 (2)$$
where ρven was blood density with a value of 1060 kg/m3, Vven denoted voxel volume, vven and represented the voxel velocity. The time frame was normalized to the individual period of end systolic time and was presented as the percentage of the end-systole (%ES). Two-tailed Student t test and Pearson correlation were performed when appropriate. P < 0.05 was considered as statistical significance.
Results
Table 1 illustrated that rTOF patients showed significant higher RVESVI (33.9 ± 7.6 cm3/m2 vs. 57.2 ± 31.2 cm3/m2, P<0.001) and RVEDVI (76.7 ± 13.3 cm3/m2 VS. 116.6 ± 44.5 cm3/m2, P<0.001) than normal volunteers. Nevertheless, rTOF group demonstrated preserved RV and LV ejection fraction (RVEF and LVEF, both P>0.05). Figure 2 displayed the time courses of KEmyo and KEven .The systolic and diastolic peak KEmyo in rTOF group were similar to normal group in both LV and RV. The KEven of LV showed no substantial difference between normal and rTOF groups. In contrast, rTOF group displayed significant higher RV KEven in diastole (0.04 ± 0.02 mJ vs. 0.07 ± 0.04 mJ, P<0.001). As illustrated in Figure 3, rTOF patients presented earlier LV myocardial diastolic time-to-peak (TTPmyo) and earlier RV TTPmyo in both systole and diastole than normal volunteers (P<0.05~0.001). For intraventricular flow, rTOF group showed earlier LV TTPven in both systole and diastole and earlier RV TTPven in systole (P<0.05~0.001, Figure 3c,d).In Figure 4a, normal volunteers presented moderate correlation between KEmyo and KEven in LV (R=0.388, P<0.05). In rTOF group, the RV KEven was correlated with RV end-diastolic volume (R=0.424, P<0.05).Discussion and Conclusions
In this study, we explored the interaction of KEmyo and KEven in both LV and RV of rTOF patients. The rTOF presented earlier TTPmyo and TTPven of KE and moderate correlation between RV KEven and RVEDV.In our study, the rTOF patient’s time to peak is earlier than normal. This finding suggested that the early TTP in myocardial and intraventricular KE may be beneficial to the rTOF. In the current work, the positive correlation between LV KEmyo and KEven in the normal group indicated the normal interaction between myocardium and intraventricular flow. The absence of this interaction in rTOF patients reflected the disordered incoherence of myocardium and intraventricular flow in a relatively early stage, i.e. with preserved global LVEF.
Previous study reported that higher intracardiac vorticity of rTOF patients could be relevant with regard to the development of RV dilation.7 In this study, the positive correlation between RV KEven and RVEDV in the rTOF group indicated that the dilated RV have impacts on the RV KEven which reflected the increased and disturbed intraventricular flow. In conclusion, from an insight of energy conversion, rTOF patients demonstrated undermined interaction between LV myocardium and intraventricular flow in an early stage. The dilated RV potentially have impacts on the RV KEven in rTOF patients.
Acknowledgements
No acknowledgement found.References
- Apitz, C., Webb, G. D., & Redington, A. N. Tetralogy of fallot. The Lancet. 2009;374(9699):1462-1471
- Arvidsson, P. M., Töger, J., Heiberg, E., et al. Quantification of left and right atrial kinetic energy using four-dimensional intracardiac magnetic resonance imaging flow measurements. Journal of applied physiology. 2013;114(10):1472-1481.
- Stankovic, Z., Allen, B. D., Garcia, J,et al. 4D flow imaging with MRI. Cardiovascular diagnosis and therapy. 2014;4(2):173.
- Sjöberg, P., Bidhult, S., Bock, J,et al.Disturbed left and right ventricular kinetic energy in patients with repaired tetralogy of Fallot: pathophysiological insights using 4D-flow MRI. European radiology. 2018;28(10):4066-4076.
- Chang, M. C., Wu, M. T., Weng, K. P,et al.Does Right Ventricular Myocardial Kinetic Energy Correlate With Pressure Overload in Repaired Tetralogy of Fallot Patients? 2017; ISMRM 25th Annual Meeting in Hawaii, The USA. Program number: 3149
- Chang, M. C., Wu, M. T., Weng, K. P,et al. Evaluate Right Ventricle-Pulmonary Artery Interaction in Patients with Repaired Tetralogy of Fallot by 4D flow-derived Kinetic Energy. 2017;ISMRM 25th Annual Meeting in Hawaii, The USA. Program number: 3222
- Hirtler, D., Garcia, J., Barker, A. J,et al. Assessment of intracardiac flow and vorticity in the right heart of patients after repair of tetralogy of Fallot by flow-sensitive 4D MRI. European radiology. 2016;26(10):3598-3607.
Figures
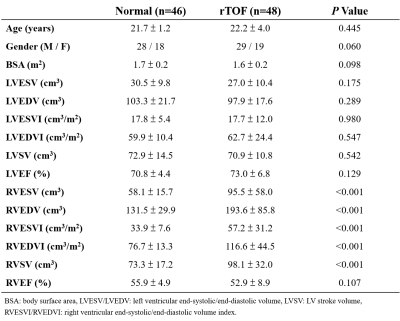
Table 1. Demographic
characteristics
of the study population.
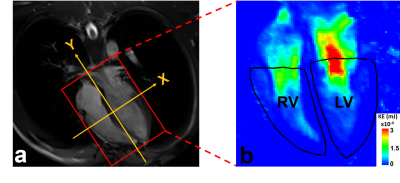
Figure
1. The
4 chamber
view of cine SSFP image (a) and the
manually determined ROIs of LV and RV on the kinetic energy map.
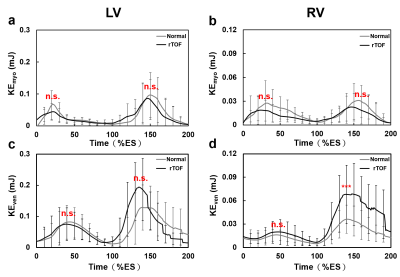
Figure
2. The
time courses of KEmyo and KEven in LV (a,c) and
RV (b,d) of
normal and rTOF
groups.
n.s.: no
significance in peak systole or diastole, ***:P
< 0.001
in peak diastole.
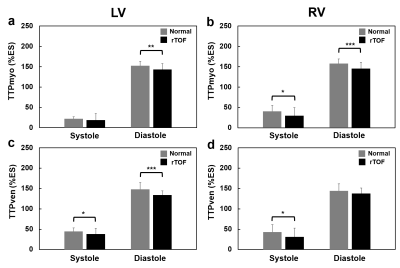
Figure
3.
The
time-to-peak (TTP) of KEmyo and KEven in LV (a,c) and
RV (b,d) at
peak systole and diastole of normal and rTOF groups. *P <
0.05, **P < 0.01, ***P < 0.001
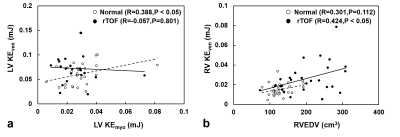
Figure
4.
The
correlation of KEmyo and KEven in LV (a) and RVEDV
and KEven
in RV (b) between normal
and rTOF groups.