1320
REACT-MD: simultaneous non-contrast-enhanced subclavian MRA and fat suppressed direct thrombus imaging (MPRAGE) with a large field-of-view1Philips Japan, Tokyo, Japan, 2Philips Healthcare, Hamburg, Germany, 3Department of Radiological Services,, Tokyo Women’s Medical University, Tokyo, Japan, 4Department of Diagnostic Imaging and Nuclear Medicine, Tokyo Women’s Medical University, Tokyo, Japan, 5Department of Clinical Radiology, Graduate School of Medical Sciences, Kyushu University, Fukuoka, Japan, 6Philips Healthcare, Best, Netherlands
Synopsis
Direct visualization of the plaques and vessel wall lesions in addition to luminal changes is of clinical importance for management of patients with atherosclerotic disease. In this work, the recently proposed REACT (Relaxation-Enhanced Angiography without Contrast and Triggering) technique was further developed and particularly optimized with Multiple Delays (REACT-MD) to simultaneously provide non-contrast-enhanced MR angiogram and MPRAGE (magnetization prepared rapid gradient echo) type images with uniform background tissue suppression over a large field of view. Initial results in patients showed great promise in detection of luminal changes and plaques for assessment of systemic atherosclerosis in one single scan.
Introduction
It is clinically desirable1 to know the location and distribution of atherosclerotic plaque assists in preprocedural planning2 and the detection of systemic atherosclerotic plaques at different arteries, such as the carotid arteries and aortic arch.Direct thrombus imaging, based on magnetization prepared rapid gradient echo (MPRAGE), is one of the most frequently-used methods for evaluating the atherosclerotic plaque3. Recently, a new 3D MPRAGE direct thrombus imaging technique with a large field-of-view (FOV), from aortic artery to internal carotid artery, enables sufficient blood suppression and robust fat suppression using improved DIXON-based gradient echo sequence (mDIXON-MPRAGE)4. Furthermore, simultaneous acquisition of MR angiography (vessel burden information) and thrombus or intraplaque hemorrhage (IPH) detection5 could be helpful because it is time-efficient without motion-related misregistration.
On the other hand, a new non-contrast-enhanced, relaxation-based, flow-independent MRA method, called Relaxation-Enhanced Angiography without Contrast and Triggering (REACT) has recently been proposed for vascular imaging in various body parts with large anatomical coverage6. REACT consists of a 3D dual-echo Dixon segmented gradient echo and magnetization preparation using a T2prep pulse and a non-selective inversion recovery (IR) pre-pulse. We hypothesised that REACT can be extended to obtain MPRAGE images in one single scan because the applied IR pulse and the sequence structure is similar to mDIXON-MPRAGE4. In this study, we attempted to develop simultaneous MRA and MPRAGE imaging with a large FOV using REACT with Multiple Delays (REACT-MD).
Methods
REACT-MD sequence:A schematic overview of the REACT-MD sequence is shown in Figure 1. It basically consists of two signal readouts by 3D Dixon dual-echo turbo field-echo (TFE) preceded by a T2prep pulse and a non-selective IR pulse [Fig.1a]. Magnetization preparation pulses were implemented to suppress signal from tissues such as muscles, nerves and organs, according to their difference in relaxation times. In detail, immediately after the T2prep pulse, an IR pulse was applied with a short inversion time (TI) to suppress tissues with short-to-intermediate T1 and T2, thus enhancing the blood-to-tissue contrast during the first signal readout for MRA [Fig.1b]. Thereafter, at the time of the blood null point, the second signal readout was carried out additionally to obtain the MPRAGE images [Fig.1a] . Consequently, REACT-MD provides MRA (phase-1) and MPRAGE (phase-2) images in one single scan without prolonging the total acquisition time. Besides, for robustness against B1 and B0 sensitivity across the entire the large-FOV, we applied a broadband offset independent trapezoid (OIT) pulse for both four T2prep refocusing pulses and the IR pulse, as already introduced for brachial plexus MR neurography and spine MR bone imaging7-10.
Experiments:
A total of 5 volunteers and 5 patients were examined on a 3.0T whole-body clinical system (Ingenia, Philips Healthcare). The study was approved by the local IRB, and written informed consent was obtained from all subjects.
(1) Parameter optimization:
To investigate an optimal inversion delay (TFE phase interval, Fig.1a) for nulling the blood signal, we targeted for an optimal TI ranging from 500 to 1000ms with 50ms increments. To quantitatively compare the effect of respective inversion times, we measured the contrast-ratio (CR) between the vessel lumen and background muscles. First, circular-shaped regions-of-interest (ROIs) were placed over the ascending aorta, bilateral common carotid arteries and bilateral subclavian arteries on the REACT MRA images [Fig.2a]. Subsequently, these ROIs were copied to the same location over the REACT-MPRAGE with respective TI images. In addition, the ROIs for muscles were also placed over the bilateral sternocleidomastoid muscles [Fig.2b]. Finally, the CR values were calculated by using average signals of all vessels and the bilateral sternocleidomastoid muscles. Furthermore, images of respective TIs were visually assessed and compared by the radiologists and technologists.
(2) Comparison with conventional sequences:
To investigate the effect of REACT-MD, we visually compared the image quality with conventional REACT and mDIXON-MPRAGE in regards to overall SNR and the presence of artifacts.
Imaging parameters for REACT-MD were; Coronal, voxel size=1.00x1.00 x1.00mm3, TFE shot-interval=4000ms, TR=4.3ms, TE1/TE2=1.52/2.8ms, flip angle=12°, NSA=1, TFE factor=50, Compressed SENSE-reduction factor=3.3, and total acquisition time=5m0s.
Results and Discussion
The optimal TI was found to be around 600ms, when CR between blood and muscle reached maximum [Fig.2c]. The quality of REACT-MD MRA and MPRAGE images was considered comparable to that of the conventional REACT MRA and mDIXON-MPRAGE, respectively. Representative images from all these techniques are shown in Figure 3. It is noteworthy that REACT-MD provided MRA and MPRAGE images in one single scan and allowed for imaging over a large FOV at 3.0T. Two clinical cases with patients with systemic atherosclerotic plaques [Fig.4] and left subclavian artery occlusion due to the presence of thrombus [Fig.5] demonstrated that multiple plaques with IPH may be clearly visualized in REACT-MD with complementary MRA on vascular morphology. The clinical information provided was at least equivalent to that obtained from the conventional sequences separately. It may even be superior owing to uniform background tissue suppression at multiple delays, the efficacy of which would need to be investigated more systematically.Conclusion
REACT-MD enables both MR angiography and MPRAGE direct thrombus imaging simultaneously, with uniform fat suppression over a large FOV in one single scan. It holds promise for assessment of systemic atherosclerosis and further clinical studies in comparison to the other state-of-the-art methods5 are warranted.Acknowledgements
No acknowledgement found.References
1. Saba L, et al. Carotid artery wall imaging: perspective and guidelines from the ASNR vessel wall imaging study group and expert consensus recommendations of the American Society of Neuroradiology. AJNR Am J Neuroradiol. 2018;39(2):E9-E31.
2. Yuan C, et al. MRI of atherosclerosis. J Magn Reson Imaging. 2004;19(6):710-9.
3. Moody AR, et al: Characterization of complicated carotid plaque with magnetic resonance direct thrombus imaging in patients with cerebral ischemia. Circulation 107:3047–3052, 2003.
4. Toyonari N, et al. Robust fat suppressed direct thrombus imaging (MPRAGE) sequence with a large field-of-view at 3T. Proc Intl Soc Mag Reson Med. 2017;25:2775.
5. Wang J, et al. Simultaneous noncontrast angiography and intraplaque hemorrhage (SNAP) imaging for carotid atherosclerotic disease evaluation. Magn Reson Med. 2013;69(2):337-45.
6. Yoneyama M, et al. Free-breathing non-contrast-enhanced flow-independent MR angiography using magnetization-prepared 3D non-balanced dual-echo Dixon method: A feasibility study at 3 Tesla. Magn Reson Imaging. 2019:16;63:137-146.
7. Yoneyama M, et al. Motion-sensitized driven-inversion (MSDI) for improvement of diffusion-prepared MR neurography (SHINKEI) in the brachial plexus. Proc Intl Soc Mag Reson Med. 2017;25:0854.
8. Yoneyama M, et al. Quantitative MR Neurography with robust fat suppression. Proc Intl Soc Mag Reson Med. 2018;26:5400.
9. Yoneyama M, et al. Robust motion-compensated lumbar spine bone imaging using 3D UTE with broadband inversion recovery pulse and k-space weighted navigator gating. Proc Intl Soc Mag Reson Med. 2019;27:0133.
10. Yoneyama M, et al. 3D broadband IR-prepared UTE bone imaging for assessment of ossification of the posterior longitudinal ligament (OPLL) in the cervical spine. Proc Intl Soc Mag Reson Med. 2019;27:2873.
Figures
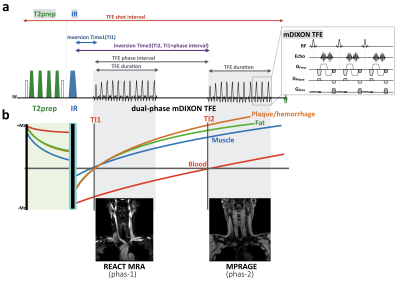
Figure 1. Scheme overview of REACT-MD sequence.
REACT consisting of a 3D DIXON-TFE with T2prep and IR pulse (a). Immediately after the T2prep pulse, an IR pulse was applied with a short TI to suppress muscle and fat (b). REACT-MD employs an additional DIXON-TFE shot at the timing with the null point of the blood (a). REACT-MD provides MRA (phase-1) and MPRAGE (phase-2) images in one single scan. For robustness against B1 and B0 inhomogeneity over a large-FOV, we applied a broadband offset independent trapezoid (OIT) pulse for both the four T2prep refocusing pulses and the IR pulse.
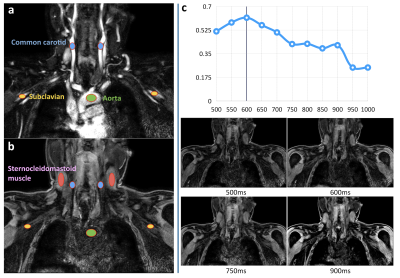
Figure 2. Inversion delay optimization for MPRAGE.
(a) To calculate the contrast-ratio, circular-shaped ROIs were placed over the ascending aorta (green), bilateral common carotid arteries (blue) and bilateral subclavian arteries (yellow) on the REACT MRA images.
(b) The ROIs were copied to same location over the REACT-MPRAGE with respective TIs. The ROIs for muscles were also placed over the bilateral sternocleidomastoid muscles (pink).
(c) The results of TI optimization. The null point of blood signals was around 600ms, and representative REACT-MD images with some TIs.
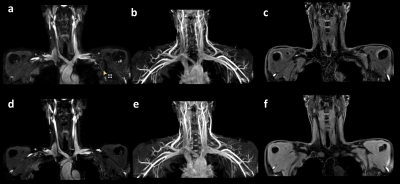
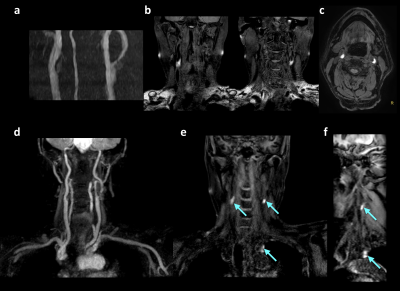
Figure 4. Representative clinical case with a patient with systemic atherosclerotic plaques.
TOF-MRA (a), 3D TSE black-blood imaging, Axial MPRAGE (c) and REACT-MD images (d-f) are shown. REACT-MD MPRAGE clearly shows multiple plaques (blue arrows) at the bilateral carotid arteries and aorta (which was not shown in 3D TSE due to fat suppression failure) in coronal (e) and sagittal (f) MPR images.
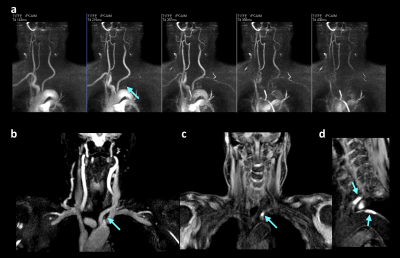
Figure 5. Representative clinical case with a patient with left subclavian artery occlusion due to the presence of thrombus.
4D phase-contrast MRA and REACT-MD MRA showed occlusion at the root of the left subclavian artery. REACT-MD MPRAGE clearly depicted multiple plaques with IPH not only at the left subclavian artery also at the aorta (blue arrows) in coronal (c) and sagittal (d) MPR images.