1209
Global longitudinal diastolic strain rate predict adverse outcomes in hypertrophic cardiomyopathyas assessed with CMR tissue tracking1West China Hospital, Chengdu, China, 2MR Collaboration, Siemens Healthineers Ltd., Shanghai, China
Synopsis
During hypertrophic cardiomyopathy (HCM), left ventricular (LV) diastolic dysfunction is regarded as one of the primary mechanisms responsible for the main adverse cardiovascular events (MACEs). Early evaluation of LV diastolic function is of great importance to risk stratification and management optimization in HCM patient populations. Our study indicated that the cardiac magnetic resonance tissue tracking (CMR-TT)–derived longitudinal global diastolic strain rate (PDSR) is a novel and easy-to-perform index for evaluating LV diastolic dysfunction and predicting adverse outcomes in HCM patient populations, which would also be beneficial for risk stratification.
Introduction
Diastolic dysfunction acts as one of the primary mechanisms responsible for the main adverse cardiovascular events (MACEs) in hypertrophic cardiomyopathy (HCM). This study aimed to explore the potential value of the global diastolic strain rate (PDSR) derived from cardiac magnetic resonance tissue tracking (CMR-TT) in predicting adverse outcomes in an HCM patient population.Methods
Ninety-eight HCM patients were enrolled and followed until a specified endpoint. The endpoint event was designated as all-cause mortality and heart failure (HF)–related mortality, including sudden cardiac death (SCD), advanced HF or HF-related death, and stroke-related death. HCM patients were divided into an obstructive subgroup (n = 44) and non-obstructive subgroup (n = 54). All CMR scans were completed in a 3-Tesla (3T) MR scanner (MAGNETOM Skyra; Siemens Healthcare, Erlangen, Germany). CMR cine images were performed using a segmented breath-hold acquisition method with fast gradient-echo readouts to eliminate image artifacts caused by B0 inhomogeneity at 3T. MR data were uploaded and analyzed on commercially available post-processing software (cvi42, Version 5.2.2; Circle Cardiovascular Imaging, Inc., Calgary, Alberta, Canada). LV global myocardial mechanics of all patients were assessed by the CMR-TT method using CMR cine images.Results
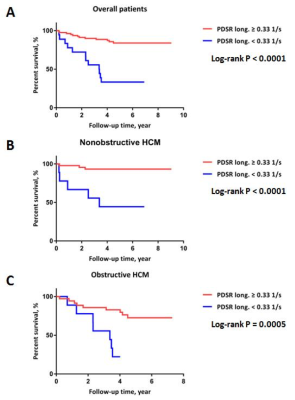
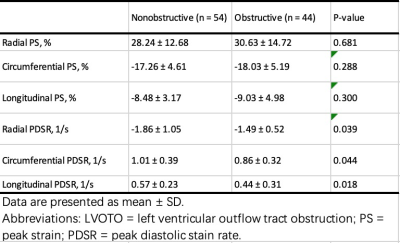
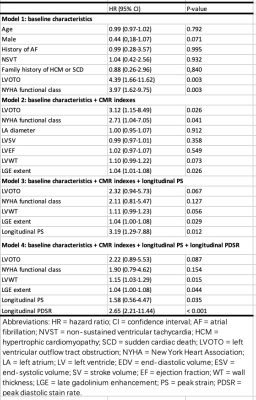
Compared with the non-obstructive subgroup, the obstructive subgroup had a declining magnitude of LV global radial, circumferential, and longitudinal peak diastolic strain rates (PDSRs) at study enrollment (all P < 0.05; Table 1). After a mean follow-up of 4.5 years, a total of 24 patients experienced MACE. Furthermore, when applying the specified cut-off value of 0.33 1/s for longitudinal PDSR, the Kaplan-Meier curve demonstrated that patients with lower longitudinal PDSRs experienced a significantly higher incidence of MACE [WS1] when compared with their counterparts among the non-obstructive, obstructive, and overall cohorts, respectively (all log-rank P < 0.05; Figure 1). Multivariable analysis demonstrated that the longitudinal PDSR remained an independent predictor of outcome despite adjusting for baseline and CMR variables (hazard ratio: 3.17, 95% confidence interval: 1.20-8.37; P < 0.05) (Table 2). [WS1]Please ensure that the intended meaning has been preserved with this edit.Discussion
Our present study had several main findings which included: 1) Patients with LV outflow tract obstruction (LVOTO) had magnitudes of global PDSR in radial, circumferential, and longitudinal directions that were worse than those of patients without LV outflow tract obstruction, indicating that the presence of LVOTO in HCM adversely impacted the progression of diastolic dysfunction; 2) During long-term follow-up, patients who experienced MACE demonstrated decreased LV global PDSR. Lower LV global PDSR was related to a higher frequency of MACE; and 3) The LV global PDSR served as an independent predictor of adverse outcomes after adjusting for other confounding factors and could be considered a novel index for risk stratification assessment in HCM patients.Conclusions
CMR-TT-derived longitudinal PDSR could be used as a novel and easy-to-perform marker for predicting adverse outcomes in HCM patients, which would also be beneficial for risk stratification. Further confirmatory studies are needed.Acknowledgements
This work was financially supported by the National Natural Science Foundation of China(81600299),1-3-5 project for disciplines of excellence of West China Hospital,Sichuan University(ZYGD18019)References
1. Seferović PM, Polovina M, Bauersachs J, Arad M, Gal TB, Lund LH, Felix SB, Arbustini E, Caforio ALP, Farmakis D, Filippatos GS, Gialafos E, Kanjuh V, Krljanac G, Limongelli G, Linhart A, Lyon AR, Maksimović R, Miličić D, Milinković I, Noutsias M, Oto A, Oto Ö, Pavlović SU, Piepoli MF, Ristić AD, Rosano GMC, Seggewiss H, Ašanin M, Seferović JP, Ruschitzka F, Čelutkiene J, Jaarsma T, Mueller C, Moura B, Hill L, Volterrani M, Lopatin Y, Metra M, Backs J, Mullens W, Chioncel O, de Boer RA, Anker S, Rapezzi C, Coats AJS, Tschöpe C. Heart failure in cardiomyopathies: a position paper from the Heart Failure Association of the European Society of Cardiology. Eur J Heart Fail. 2019;21(5):553-76.
2. Chamsi-Pasha MA, Zhan Y, Debs D, Shah DJ. CMR in the evaluation of diastolic dysfunction and phenotyping of HFpEF: Current role and future perspectives. JACC Cardiovasc Imaging. 2019. pii: S1936-878X(19)30373-0.
Figures