1191
Detection of radiation brain injury in patients with nasopharyngeal carcinoma: A comparative study of DTI, DKI and MAP-MRI1Deptpartment of Radiology, SUN YAT-SEN Memorial Hospital, SUN YAT-SEN University, Guangzhou, China, 2MR Scientific Marketing, Siemens Healthcare, Guangzhou, China, 3department of NEUROLOGY, Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China, 4MR Scientific Marketing, Siemens Healthineers, Shanghai, China, 5Shanghai Key Laboratory of Magnetic Resonance, East China Normal University, Shanghai, China, 6Sun Yat-sen Memorial Hospital, Sun Yat-sen University, Guangzhou, China
Synopsis
Mean apparent propagator (MAP)-MRI, which builds a powerful analytical framework based on the random motion distribution of real water molecules, can more accurately and comprehensively characterize microstructure features of brain tissues than conventional diffusion imaging. This study investigated the application of MAP-MRI in the early diagnosis of radiation-induced brain injury in patients with nasopharyngeal carcinoma, compared with diffusion tensor imaging (DTI) and diffusion kurtosis imaging (DKI).
Introduction
Radiotherapy or radiochemotherapy is widely used in the treatment of Nasopharyngeal carcinoma (NPC) [1]. However, it often induces aggravated radiation-induced brain injury. Generally, early radiation brain damage is manifested as a small edema focal of the occipital lobe. Early diagnosis and treatment of radiation-induced brain injury is very important, which is related to the efficacy of chemoradiotherapy in patients. Advanced diffusion imaging can be used as an early diagnostic method of radiation-induced brain injury. This study used diffusion tensor imaging (DTI), diffusion kurtosis imaging (DKI) and Mean apparent propagator (MAP)-MRI to quantitatively detect early radiation-induced brain injury in patients with NPC. In addition, the performance of these three diffusion methods was compared.Methods
A total of 33 patients (average age 53.02 ± 11.25 years, 24 males, 9 females) previously histopathologically confirmed NPC and 12 normal controls (NCs) (average age 53.02 ± 11.25 years, 7 males, 5 females) were recruited. All patients underwent MRI scan on a 3T MR scanner (MAGNETOM Skyra, Siemens Healthcare, Erlangen, Germany). T1WI, T2WI, and dynamic contrast-enhanced T1WI were acquired for morphological diagnosis in conventional MRI examinations. An axial DSI sequence, a q-space Cartesian grid sampling procedure with 128 diffusion gradient directions and sixteen b-values (bmax = 2000 s/mm2), were performed to obtain diffusion-weighted (DW) data. The sequence parameters were as follows: repetition time (TR) = 4900 ms, echo time (TE) = 93 ms, field of view (FOV) = 220 × 220 mm2; matrix size = 110 × 110; slice thickness = 4 mm, acquisition time = 12:17 min. All DW data were calculated by the software called NeuDiLab, which was developed in-house based on an open-source tool DIPY (Diffusion Imaging In Python, http://nipy.org/dipy). And the parameters of the three diffusion methods were obtained. The MAP-MRI parameters included return-to-origin probability (MAP-RTOP), return to axis probability (MAP-RTAP), return to plane probability (MAP-RTPP), mean squared displacement (MAP-MSD) and Q-space inverse variance (MAP-QIV). The DTI parameters included axial, radial, and mean diffusivity (DTI-AD, DTI-RD, DTI-MD) and fractional anisotropy (DTI-FA). The DKI parameters included radial, axial, and mean kurtosis (DKI-RK, DKI-AK, DKI-MK), DKI-MD, DKI-AD, DKI-RD, and DKI-FA. For each patient, the maximum cross-sectional area of the enhanced edema focal on the T2WI images was manually drawn as the region of interest (ROI) by visual inspection, and then the location of ROI was copied to all obtained parameters to calculate the corresponding average values. Differences in all diffusion parameters between NPC patients and NCs were compared using the Mann-Whitney U test, and the diagnostic effectiveness was evaluated by receiver operating characteristic (ROC) curve analysis.Results
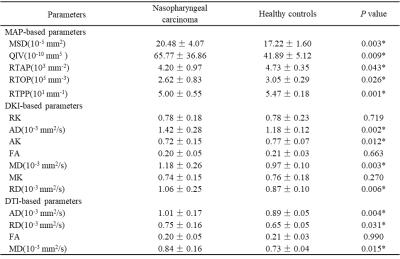
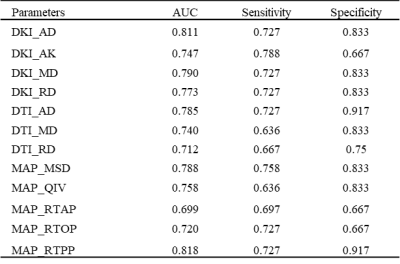
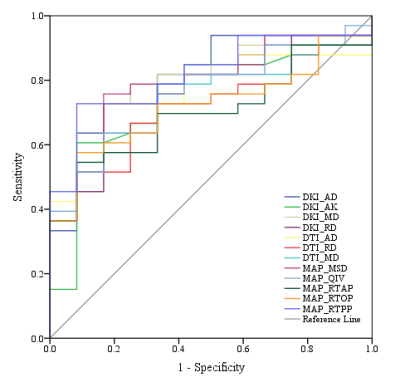
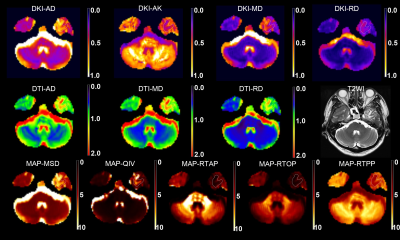
As shown in Table 1, between NPC patients and NCs, there were significant differences in MAP-MRI-based MSD, QIV, RTOP, RTAP, RTPP, DTI-based AD, RD, MD, and DKI-based AK, MD, AD, RD (p<0.05). One representative case is shown in Figure 1. Figure 2 and Table 2 demonstrated that the AUCs of MAP-MSD, MAP-QIV, MAP-RTOP, MAP-RTAP, MAP-RTPP, DTI-AD, DTI-RD, DTI-MD, DKI-AK, DKI-MD, DKI-AD, and DKI-RD were all above 0.7, and the MAP-RTPP achieved the highest AUC (0.818) and specificity (0.917) in diagnosis of radiation brain injury.Discussion and Conclusion
Radiation-induced brain injury is a serious complication of head and neck tumor after radiotherapy, which is aggravated with the treatment course. Therefore, it is essential to find a better non-invasive method for early diagnosis. This study used three advanced diffusion imaging (DTI, DKI and MAP-MRI) to quantitatively diagnosis the edema focal induced by radiochemotherapy, which breaks through the limitation that traditional MRI can only use T1 and T2 weighted images for clinical rough morphological diagnosis of radiation brain injury[2]. Compared to DTI and DKI, MAP-MRI is a more potential method for the early diagnosis of radiation brain damage caused by radiotherapy of nasopharyngeal carcinoma.Acknowledgements
No acknowledgement found.References
1. Cai J, Cheng J, Li HA, et al. Nomogram for the prediction of cerebrovascular disease among patients with brain necrosis after radiotherapy for nasopharyngeal carcinoma. Radiother Oncol. 2019 Mar;132:34-41.
2. Alexandru V. Avram , Joelle E. Sarlls , Alan S. Barnett. Clinical feasibility of using mean apparent propagator (MAP) MRI to characterize brain tissue microstructure. NeuroImage 2015