1177
Preoperative evaluation of multimodal spinal MRI in patients with acute traumatic spinal cord injury1Radiology, Union Hospital, Wuhan, China, 2orthopedics, Union Hospital, Wuhan, China, 3Philips Healthcare, Beijing, China
Synopsis
Baseline MRI was recommended in acute spinal cord injury for clinical decision making and outcome prediction. The study presented a new quantitative method for evaluating the spinal cord severity to grade the retained fiber tracks by zoom DTI in pre-operation. For patients with ASIA A, no ASIA grade got promoted in FTClass A1 with completely fibers interruption and 3 out of 6 patients converted to C within 6-month follow-up in FTclass A2 with partially retention. The retained spinal cord fibers were critical for postoperative functional recovery. Multimodal MRI, especially accurate DTI provide potential quantitative predictive indicators for prognosis.
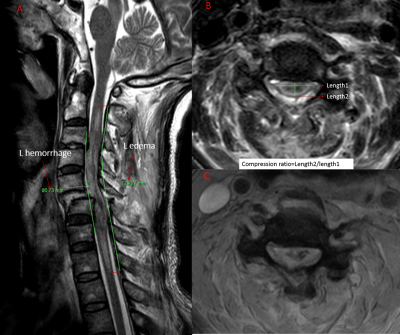
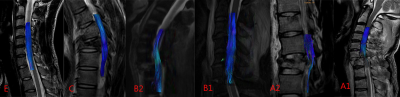
Methods: The multimodal MRI data was acquired with a 3.0T MR scanner (Ingenia, Philips Healthcare, the Netherlands), which included conventional T2-weighted imaging (T2w) in sagittal (SAG) and transverse (TRA) plan, T1-weighted in SAG, diffusion tensor imaging (DTI) in TRA, and multi-echo FFE (mFFE) with scan parameters shown in Table 1. Conventional T2w and T1w were used to evaluate the edema and contusion of the spinal cord. For mFFE, a multi-echo T2* sequence was applied to accurately assess spinal cord injury and hemorrhage. For DTI data, Zoom imaging was used to reduced FOV and artefacts [2]. Fiber tractography (FT) was used to assess the fiber bundle sparse, transition and fracture. We measured the length of edema and hemorrhage [3] and compression ratio (Fig 1) [4] on IntelliSpace Discovery (Philips Healthcare, the Netherlands), and classified the severity of fibers damage as in Fig 2. The American Spinal Injury Association (ASIA) classification was performed to evaluate the degree of spinal cord injury before and after surgeries.
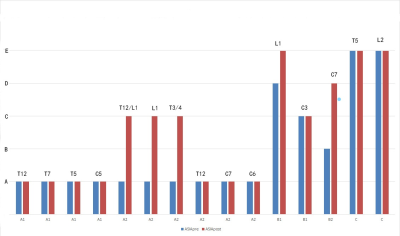
Results: Fifteen patients (5 cervical lumbar and 10 thoracolumbar; 13 male and 2 female, mean age: 48.8±15.8 years) with baseline and 6-month follow-up after operations were included. Preoperative ASIA (ASIApre) was evaluated within three days of injury and Postoperative ASIA (ASIApost) was evaluated 6 months after operation. The length of edema and hemorrhage correlated with ASIApre and ASIApost (edema R2=0.664 and 0.540 respectively, p<0.05; hemorrhage R2=0.658 and 0.672 respectively, p<0.01, Spearman). The FTclass strongly correlated with ASIApre and ASIApost (R2=0.867 and 0.860 respectively; p<0.01, spearman, Table 2). For the patients of ASIApre A and FTclass A1, 3 patients had no changes 6 months after operations, 1 patient died in 4 weeks after operation. As the patients with ASIApre A and FTclass A2, 3 patients recovered to C after operations and 2 cases retained A (injury level were C6 and C7), 1 patient (T12) retained as A after operation while muscle strength was improved. The result showed that the retained fibers were important for motor and sensation recovery. The study could explain that why some patients of the ASIA A had not recovered at all while some others had some improvements in motor and sensation function.
Conclusion: The severity of acute traumatic spinal cord injury was associated with edema and hemorrhage. The retention of spinal cord fibers were critical for postoperative functional recovery. Accurate assessment of spinal cord injury (with edema, contusion, and hemorrhage) and classification the fiber bundles before operation could provide accurate diagnostic information and treatment guidance for clinicians, and become potential quantitative predictive indicators for prognosis.
Acknowledgements
No acknowledgement found.References
[1] Fehlings M G, Tetreault L A, Wilson J R, et al. A Clinical Practice Guideline for the Management of Acute Spinal Cord Injury: Introduction, Rationale, and Scope[J]. Global Spine Journal. 2017, 7(3_suppl): 84S-94S.
[2] Yokohama T, Iwasaki M, Oura D, et al. The Reliability of Reduced Field-of-view DTI for Highly Accurate Quantitative Assessment of Cervical Spinal Cord Tracts[J]. Magnetic Resonance in Medical Sciences. 2019, 18(1): 36-43.
[3] Aarabi B, Sansur C A, Ibrahimi D M, et al. Intramedullary Lesion Length on Postoperative Magnetic Resonance Imaging is a Strong Predictor of ASIA Impairment Scale Grade Conversion Following Decompressive Surgery in Cervical Spinal Cord Injury[J]. Neurosurgery. 2017, 80(4 ): 610-620.
[4] Karpova A, Arun R, Davis A M, et al. Reliability of Quantitative Magnetic Resonance Imaging Methods in the Assessment of Spinal Canal Stenosis and Cord Compression in Cervical Myelopathy[J]. Spine. 2013, 38(3): 245-252.
Figures