1149
Classification of Spinal Metastases Coming from Different Primary Cancer Origin by Using Quantitative Radiomics Analysis with Multi-Class SVM1Department of Radiology, Peking University Third Hospital, Beijing, China, 2Department of Radiological Sciences, University of California, Irvine, CA, United States
Synopsis
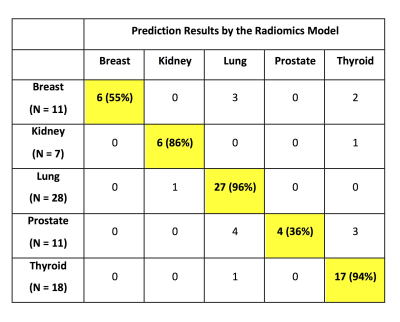
For patients suspected to have spinal metastasis, a confirmed pathological diagnosis is needed to proceed with appropriate treatment. This study applied quantitative radiomics to differentiate 5 groups of patients with metastatic cancers in the spine, including 28 lung, 11 breast, 7 kidney, 11 prostate and 18 thyroid. The analysis was done on post-contrast images. A total of 107 features, including 32 first order and 75 texture, were extracted for each case by using PyRadiomics. The group differentiation was done by using multi-class support vector machine (SVM). The overall accuracy was 80%, with the highest accuracy of 27/28=96% for lung mets.
Introduction
Patients presenting with pain in the spine are often suspected to have lesions compressing the spinal cord, and MRI is usually performed for diagnosis. The most common malignancy in the spine is metastatic cancer, and approximately 30% of patients present with an unknown primary [1-3]. In these patients, a final diagnosis is needed to proceed with treatment. If the origin of the cancer in the spine can be accurately predicted based on imaging or biomarkers, this can narrow the search and help determine the most appropriate method to locate the primary tumor without the need of performing invasive spinal biopsy. In Western world with established health care systems, PET/CT is the most commonly used imaging for diagnosis of primary cancer and whole-body staging when the metastatic cancer in the spine is suspected. However, the patient may have to wait for insurance approval and delay the diagnosis. In the developing countries, PET/CT and the [18F]-FDG tracer are limited and very expensive, and thus this exam may not be available to many patients. Other cheaper imaging examinations that can provide a cost-effective management approach will be very helpful. Among all patients presenting with spinal pain with an unknown primary cancer site, lung metastasis is the most prevalent [3]. Other cancers, including breast, kidney, prostate and thyroid, are also common primary that can metastasize to the spine. The purpose of this study is to apply quantitative radiomics analysis and multi-group classification methods to differentiate these 5 different primary cancers metastasizing to the spine.Methods
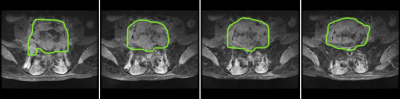
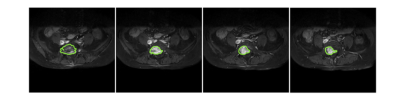
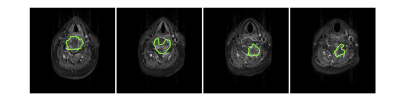
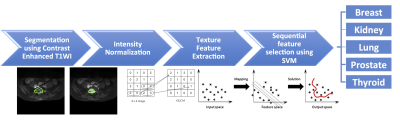
The cases were identified by a retrospective review of our spinal clinical MRI database. Only patients who were conformed to have these 5 primary cancers were analyzed, including Lung (N=28), Breast (N=11), Kidney (N=7), Prostate (N=11) and Thyroid (N=18). Other primary cancers, such as liver, colorectal and stomach cancers were also found, but since the case number was too small, not included in the analysis. MR scans were performed on a 3T Siemens or a 3T GE scanner, with a comparable protocol. After the abnormal segments in the spine were identified, T1-weighted contrast-enhanced MRI was performed on the axial view to cover the entire abnormal region. The analysis was done based on the post-contrast images. A radiologist manually outlined the tumor ROI on each slice, and the ROI’s from all slices containing the tumor were combined to generate a 3D tumor mask. Three case examples are shown in Figures 1 to 3. The radiomics analysis was performed using the PyRadiomics, the open-source radiomics library written in python. A total of 107 features, including 32 first order and 75 texture, were extracted for each case. For differentiation among the 5 primary cancer groups, sequential feature selection was done by constructing multiple support vector machine (SVM) classifiers. The features with the highest importance were selected to build the final SVM classification model with Gaussian kernel. 10-fold cross-validation was applied to test the model performance. The radiomics analysis flow chart is shown in Figure 4.Results
During the feature selection process, 6 features with the highest importance were selected to build the final SVM classification model. They are: 1) GLCM autocorrelation, 2) GLSZM Small Area High Gray Level Emphasis, 3) GLCM difference entropy, 4) GLCM cluster shade, 5) GLRLM long run emphasis, and 6) GLDM gray level non uniformity. The multi-group classification results are shown in Table 1. The overall accuracy was 80% (60 correct out of 75). The accuracy was very high for lung cancer (27/28=96%), thyroid cancer (17/18=94%), and kidney cancer (6/7=86%), only missing one case in each group. The accuracy for the breast cancer was 6/11 (55%), with 3 mis-diagnosed as lung mets and 2 as thyroid mets. The lowest accuracy was found for the prostate cancer, only 4/11 (36%), with 4 mis-diagnosed as lung mets and 3 as thyroid mets.Discussion
In this study, we performed quantitative radiomics analysis to extract features from post-contrast images to diagnose metastatic cancer in the spine coming from different primary site of origin. The appearance of many spinal lesions was similar on conventional MRI [4-8], and could not be diagnosed with visual examination. Osteolytic lesion was the most common abnormality seen in the spine, and metastatic lesion was often accompanied with soft tissue mass. Early detection and correct diagnosis of metastasis is critical, as the spread cancer can be quickly treated and controlled. Patients without a known history of cancer often seek medical attention due to nerve compression and back pain. When metastatic cancer was suspected, finding and confirming the primary lesion became the most important task for treatment planning [9]. As lung mets are the most common primary, if it is suspected, a CT scan can be performed quickly at a low cost, without having to wait for approval of expensive and limited PET/CT. In this study we only analyzed the post-contrast images, not the enhancement maps by subtracting the pre-contrast images. In a recent study we further analyzed the dynamic-contrast-enhanced MRI, which could be used to quantitatively evaluate the percent enhancement as well as the vascular properties [10]. Nonetheless, it required a special imaging protocol and not commonly done as a clinical routine. The radiomics analysis can extract detailed information from post-contrast images, and easily implemented in a clinical setting. The high accuracy for diagnosis of lung mets is very helpful, so the patients can be diagnosed quickly with CT. When more cases are available for training, the accuracy is expected to be improved, and hopefully to the level that can developed as a clinical product to help management of patients with spinal metastases.Acknowledgements
This study was supported in part by the National Natural Science Foundation of China (81971578, 81701648), the Key Clinical Projects of the Peking University Third Hospital (BYSY2018007), and NIH R01 CA127927.References
[1]. Sciubba DM, Petteys RJ, Dekutoski MB, et al. Diagnosis and management of me- tastatic spine disease. J Neurosurg Spine 2010;13:94–108.
[2]. Robson P. Metastatic spinal cord compression: a rare but important complication of cancer. Clin Med (Lond) 2014;14:542–5.
[3]. Piccioli A, Maccauro G, Spinelli MS, Biagini R, Rossi B. Bone metastases of unknown origin: epidemiology and principles of management. J Orthop Traumatol 2015;16:81–6.
[4]. Erlemann R, Reiser MF, Peters PE, Vasallo P, Nommensen B, Kusnierz-Glaz CR, et al. Musculoskeletal neoplasms: static and dynamic Gd-DTPA enhanced MR imaging. Radiology 1989;171:767–73.
[5]. Hermann G, Abdelwahab LF, Miller TT, Klein MJ, Lewis MM. Tumour and tumour- like conditions of the soft tissue: magnetic resonance imaging features differ- entiating benign from malignant masses. Br J Radiol 1992;65:14–20.
[6]. Moulton JS, Blebea JS, Dunco DM, Braley SE, Bisset 3rd GS, Emery KH. MR imaging of soft-tissue masses: diagnostic efficacy and value of distinguishing between benign and malignant lesions. Am J Roentgenol 1995;164:1191–9.
[7]. May DA, Good RB, Smith DK, Parsons TW. MR imaging of musculoskeletal tumors and tumor mimickers with intravenous gadolinium: experiences with 242 patients. Skeletal Radiol 1997;26:2–15.
[8]. Kim HJ, Ryu KN, Choi WS, Choi BK, Choi JM, Yoon Y. Spinal involvement of he- matopoietic malignancies and metastasis. differentiation using MR imaging Clin Imaging 1999;23:125–33.
[9]. Ortiz-Ramón R, Larroza A, Ruiz-España S, Arana E, Moratal D. Classifying brain metastases by their primary site of origin using a radiomics approach based on texture analysis: a feasibility study. Eur Radiol. 2018;28(11):4514-4523.
[10]. Lang N, Zhang Y, Zhang E, et al. Differentiation of spinal metastases originated from lung and other cancers using radiomics and deep learning based on DCE-MRI. Magn Reson Imaging. 2019 Feb 28. pii: S0730-725X(18)30672-6. doi: 10.1016/j.mri.2019.02.013. [Epub ahead of print]
Figures