1148
Abnormal [18F]FDG PET/MRI Findings in Paraspinal Structures of Patients with Suspected Cerebrospinal Fluid Leak1Stanford University, Stanford, CA, United States, 2Stanford University, Palo Alto, CA, United States, 3Stanford University, Redwood City, CA, United States
Synopsis
Six patients with suspected cerebrospinal fluid leak but in whom no site of leakage had been identified and six controls underwent simultaneous, whole-body [18F]FDG PET/MRI imaging. Increased [18F]FDG uptake was found in paraspinal structures in all six patients and was significantly greater than in the corresponding areas of controls. Temporary but significant relief in symptoms resulted from blood patches placed at locations coinciding with PET/MRI abnormalities.
INTRODUCTION
The most characteristic symptom of a CSF leak is persistent headache that worsens when upright and improves with recumbency (orthostatic headaches).1 Unfortunately, no one diagnostic test can consistently exclude the diagnosis of CSF leak or identify the site(s) of leakage.2 Misdiagnosis is common, preventing proper treatment as the symptoms are often mistaken for those of other diseases, such as postural orthostatic tachycardia syndrome or new daily persistent headache.3,4 The underlying sensitivity of MRI and CT myelography remains unknown. In this report, we hypothesized that [18F]FDG PET, coupled with the high spatial and contrast resolution of MRI, could identify inflammation around the sites of CSF leak due to its pro-inflammatory properties.5METHODS
IRB approval was obtained. Six patients were included who were suspected to be suffering from CSF leak and who presented with orthostatic headache. They had received standard-of-care imaging methods (including CT myelogram), without identifying a CSF leak. Six controls were also recruited. Subjects were imaged using a GE SIGNA PET/MRI system (time-of-flight PET; 3.0T bore; 4-8 min/bed position) from head to toe. One hour after a 10-mCi injection of [18F]FDG, we performed a whole-body PET/MRI scan of subjects (8-10 consecutive imaging stations). PET and MRI raw data were reconstructed using algorithms equipped in the scanner.6,7In each station, we conducted 3D axial liver imaging with volume acceleration-flexible (TR:4.6ms, TE:1.8ms, resolution:1.3x1.3x3.4mm, flip angle:15°) and 2D axial T2-weighted fast-spin-echo with two-point Dixon fat-water separation (TR:7.6s TE:93.3ms, resolution:1.5x1.5x4mm, echo train length:15). For one or two imaging stations where we suspected CSF leaks based on the patient’s history, we additionally ran the following two sequences for high-resolution imaging: 3D axial double-echo-in-steady-state (DESS) with water-only excitation (TR:18.7ms, TE:8.1ms, resolution:0.8x0.8x2mm, flip angle:30°) and 3D coronal motion-sensitized-driven-equilibrium (MSDE) fast-spin-echo sequence (CUBE) with two-point Dixon fat-water separation (TR:2.5s, TE:71.8ms, resolution: 1.4x1.4x1.4mm echo train length:80). For MRI signal acquisition, a 16-channel head-neck coil, an integrated spine coil, and two 32-channel anterior body array coils were employed.
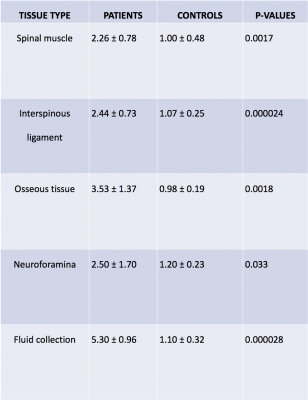
Data analysis: Abnormal [18F]FDG hotspots were identified, and maximum standardized uptake values (SUVmax) were measured using image analysis software (Horos v.3.3.5). Hotspots were categorized into 5 types: paraspinal muscle, interspinous ligament, osseous tissue, neuroforamina, and fluid. SUVmax measurements of each type were compared with SUVmax of corresponding areas in controls using a two-sided Mann-Whitney U-test (P-value<0.05 considered significant).
RESULTS
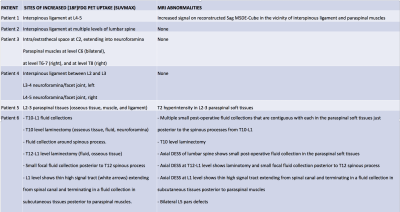
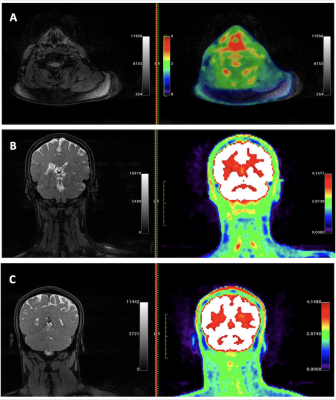
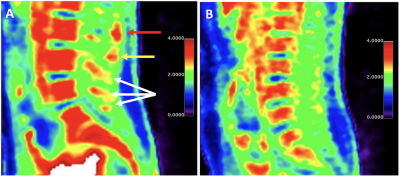
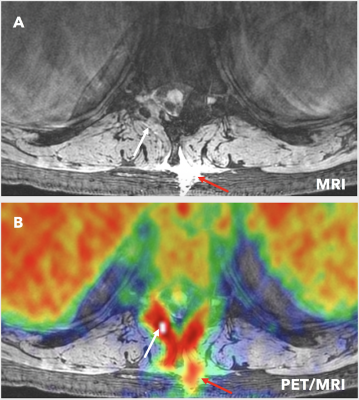
Abnormal [18F]FDG PET/MRI findings: In all six patients, abnormally increased uptake of [18F]FDG was found in paraspinal structures at various levels of the spine (Figure 1). However, only 3 patients showed MRI abnormalities, which were in the same region of the PET abnormalities (Figure 1). The [18F]FDG SUVmax in lesions from the patients showed a higher mean value than the corresponding areas from controls in all tissue types (Figure 2). SUVmax of the abnormal lesions in the patient group ranged from 1.148 to 6.565, while SUVmax of the corresponding tissues in controls ranged from 0.416 to 2.893. A Mann-Whitney U-test comparing these two groups indicated a significant difference.Blood-patch treatment outcome: Epidural blood-patching was performed at multiple levels for three patients based on information from standard-of-care diagnostic methods. Two patients underwent epidural blood-patching at the sites covering abnormalities identified by our study and reported temporary improvement in symptoms significantly greater than previous blood-patches. However, the other patient whose blood-patch sites marginally included the PET/MRI abnormalities reported no symptomatic improvement.
Figs. 3-5 present different cases of abnormally increased [18F]FDG uptake in patients: in cervical paraspinal muscles (Fig. 3), at the level of the interspinous ligament in the lumbar spine (Fig. 4A), and in areas corresponding to fluid, neuroforamina, and osseous tissue (Fig. 5). Asymptomatic controls did not show areas of focally increased [18F]FDG uptake in these regions (Fig. 4B). Note that the cases in Figs. 3 and 4 show no abnormal MRI signal change.
DISCUSSION
While other nuclear medicine approaches such as radioisotope cisternography have been used to identify CSF leaks, to our knowledge neither [18F]FDG PET nor simultaneous PET/MRI have been used for this purpose until now.8 In the case of CSF leak, extradural CSF fluid may irritate and inflame tissues outside of the nervous system5 thus providing a mechanism for PET detection using [18F]FDG as a tracer. This irritation is reflected clinically in studies of patients with chronic CSF leaks following accidental dural puncture, who report much higher rates of spinal pain at the site of CSF leak than control patients who underwent epidural injection without dural puncture.9,10 Such inflammatory lesions have increased metabolism and energy requirements and become more glucose-avid than normal tissues, which can be imaged by PET using a glucose analog radiotracer such as [18F]FDG.11,12,13 Simultaneous, time-of-flight PET/MRI could be a more useful tool in this context than a single use of [18F]FDG PET. In our results, more abnormalities were found with [18F]FDG PET than 3T MRI, which suggests [18F]FDG PET may be better suited than MRI for the detection of early inflammatory changes due to CSF leak.CONCLUSION
Increased [18F]FDG uptake was observed on PET in the paraspinal tissues of patients with suspected CSF leak. Our results suggest [18F]FDG PET/MRI is sensitive to abnormalities potentially due to CSF leak, which are not visible on standard-of-care diagnostic imaging modalitiesAcknowledgements
We would like to thank Dawn Holley and Harsh Gandhi, PET/MRI technologists, for their assistance in acquiring the images.References
1. Schievink WI. Spontaneous Spinal Cerebrospinal Fluid Leaks and Intracranial Hypotension. JAMA: The Journal of the American Medical Association 2006;295:2286–96.
2. Kranz PG, Malinzak MD, Amrhein TJ, et al. Update on the Diagnosis and Treatment of Spontaneous Intracranial Hypotension. Curr Pain Headache Rep 2017;21:37.
3. Mokri B. Spontaneous low pressure, low CSF volume headaches: spontaneous CSF leaks. Headache 2013;53:1034-53.
4. Schievink WI. Misdiagnosis of spontaneous intracranial hypotension. Arch Neurol 2003;60:1713-8. 5. Schneider UC, Schiffler J, Hakiy N, et al. Functional analysis of Pro-inflammatory properties within the cerebrospinal fluid after subarachnoid hemorrhage in vivo and in vitro. J Neuroinflammation 2012;9:28. 6. Sekine T, Buck A, Delso G, et al. Evaluation of Atlas-Based Attenuation Correction for Integrated PET/MR in Human Brain: Application of a Head Atlas and Comparison to True CT-Based Attenuation Correction. J Nucl Med 2016;57:215-20.
7. Ahn S, Ross SG, Asma E, et al. Quantitative comparison of OSEM and penalized likelihood image reconstruction using relative difference penalties for clinical PET. Phys Med Biol 2015;60:5733-51.
8. Monteith TS, Kralik SF, Dillon WP, et al. The utility of radioisotope cisternography in low CSF/volume syndromes compared to myelography. Cephalalgia 2016;36:1291-5.
9. Webb CA, Weyker PD, Zhang L, et al. Unintentional Dural Puncture with a Tuohy Needle Increases Risk of Chronic Headache. Anesthesia and Analgesia 2012;115:124–32.
10. Ranganathan P, Golfeiz C, Amy L. Chronic Headache and Backache Are Long-Term Sequelae of Unintentional Dural Puncture in the Obstetric Population. Journal of Clinical Anesthesia 2015;27:201–6. 11. Behera D, Jacobs KE, Behera S, et al. (18)F-FDG PET/MRI can be used to identify injured peripheral nerves in a model of neuropathic pain. J Nucl Med 2011;52:1308-12.
12. Catalano OA, Masch WR, Catana C, et al. An overview of PET/MR, focused on clinical applications. Abdom Radiol (NY) 2017;42:631-44.
13. Cipriano PW, Yoon D, Gandhi H, et al. (18)F-FDG PET/MRI in Chronic Sciatica: Early Results Revealing Spinal and Nonspinal Abnormalities. J Nucl Med 2018;59:967-72.
Figures