1092
Cardiac Diffusion Tensor MRI Using M2-gSlider with a Real-Time Slice Tracking Respiratory Navigator1Cardiovascular Research Center, Massachusetts General Hospital, Charlestown, MA, United States, 2Department of Medicine, Harvard Medical School, Boston, MA, United States, 3Martinos Center for Biomedical Imaging, Massachusetts General Hospital, Charlestown, MA, United States, 4Department of Radiology, Harvard Medical School, Boston, MA, United States, 5Cardiovascular Institute, Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ, United States, 6Department of Computer Science, University of São Paulo, São Paulo, Brazil
Synopsis
Free-breathing isotropic cardiac diffusion tensor MRI (DT-MRI) of the left ventricle can be performed using second moment (M2) motion compensated spin echo encoding and generalized slice dithered enhanced resolution (gSlider). This technique provides substantial improvements in spatial resolution and consequently in the accuracy of diffusion-based indices. However, M2-gSlider’s RF slice encoding is susceptible to through-slice motion, limiting the maximal improvement in slice resolution. Here, we evaluate the addition of a slice tracking respiratory navigator (NAV) to prospectively adjust slice position in real-time. M2-gSlider-NAV was validated in healthy volunteers and tested in a patient with a history of myocardial infarction.
INTRODUCTION
Recent work has shown that combining second-order gradient moment nulling (M2) and generalized slice dithered enhanced resolution (gSlider) allows isotropic in vivo cardiac diffusion Tensor MRI (DT-MRI) [1]. M2-gSlider enabled free-breathing isotropic (~2.5 mm) DT-MRI acquisition of the entire left ventricle (LV), demonstrating a nominal through-plane increase in spatial resolution by more than three times. This isotropic resolution improved analysis and visualization of fiber architecture in an “unfolded” representation, depicting both the circumferential and longitudinal myocardial microstructure. However, M2-gSlider RF slice encoding is susceptible to through-slice motion due to its inherent reliance on 2D slice selection and lack of 3D Fourier phase encoding. Consequentially, the actual improvement in slice resolution can be diminished in the presence of through-plane respiratory motion. Here we demonstrate a slice tracking respiratory navigator (NAV) capable of prospectively adjusting slice position in real-time in combination with M2-gSlider, and show marked improvement in resulting image quality.METHODS
Pulse Sequence Design: M2 compensated diffusion gradients were designed using a symmetric gradient shape insensitive to the accuracy of the refocusing pulse [1] (Fig. 1). The gSlider RF and slice selective pulses were optimized to reduce RF duration, improve slice dither profile, and reduce SAR using an application-specific VERSE design [1]. Optimized slice interleaving was performed to ensure signal recovery (4 RR) before adjacent slices were acquired. Asymmetric regional saturation bands reduced the FOV and minimized the readout duration while decreasing susceptibility distortion and echo time. A spin echo NAV with intersecting excitation and refocusing planes was placed perpendicular to the diaphragm and away from the heart to avoid saturation artifact.In Vivo Study: Four healthy volunteers and one patient with a history of myocardial infarction were imaged on a 3T scanner (Siemens Prisma) for 1.5 hours using M2-gSlider-NAV DT-MRI (TR = 10 RR, TE = 81 ms, in-plane resolution = 2.5 mm x 2.5 mm, slice thickness = 2.5 mm [RF slab thickness = 12.5 mm, gSlider factor = 5], outer volume suppression with asymmetric saturation bands, 1 b = 0 and 10 b = 500 s/mm2 diffusion directions, 10 averages, Navigator window = 12 mm) under free-breathing conditions. The entire LV was imaged in short-axis slices without gaps. The Siemens clinical spine and chest array coils were used for all acquisitions.
Image Analysis: For each subject, we computed a number of diffusion-based indices, including mean diffusivity (MD), fractional anisotropy (FA), helix angle (HA), and helix angle transmurality (HAT). An unfolded representation of the LV wall was generated by projecting 90 radial scanlines [2] 4 degrees apart, from the center at the LV cavity, at each level from apex to base, using the anterior LV-RV junction as the starting point of unfolding. The diffusion-based indices were mapped onto the unfolded representation and averaged across transmural depth. Spatiotemporal registration (STR) motion correction was applied to improve in-plane alignment of diffusion eigensystem components [2].
RESULTS
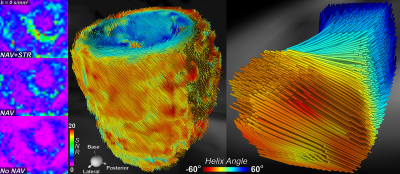
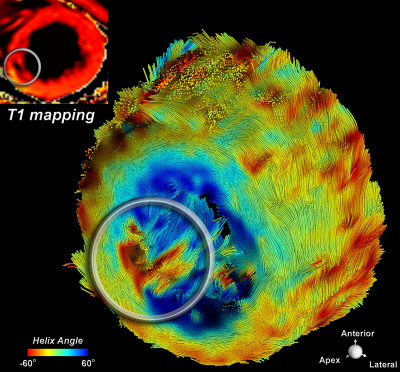
With addition of the navigator to the M2-gslider sequence there was an improvement in the alignment of the acquired images, resulting in improved morphologic definition of the LV (Fig.1). With the use of the navigator there was a more than two-fold improvement in SNR. The highest quality images were obtained when both navigator and STR were employed. Fiber tractography derived from these data demonstrated a coherent distribution of myofibers in healthy volunteers (Fig.2), as well as local disruption of fiber architecture in the region of the myocardial infarction (Fig.3). Diffusion-based indices for normal volunteers and the patient with a history of MI are shown in Figure 4.CONCLUSION
Slice-following M2-compensated diffusion EPI enables imaging of the beating heart without motion artifact while simultaneously tracking and canceling respiratory motion. The integration of a real-time slice tracking respiratory navigator to the M2-gSlider acquisition has yielded improvements in SNR and in the definition of local variability in the 3D myofiber continuum. The integration of SMS acceleration will enable this technique to be translated to the clinical setting.Acknowledgements
NIH R01HL131635
NIH R21EB024701
References
[1] Nguyen C, Reese TG, Liao C, Kostis WJ, Jackowski MP, Setsompop K, Mekkaoui C. Free Breathing Isotropic Cardiac Diffusion Tensor MRI of the Left Ventricle Using M2-gSlider: Unfolding the Fiber Architecture of the Human Heart, ISMRM 2019.
[2] Mekkaoui C, Reese TG, Jackowski MP, Cauley SF, Setsompop K, Bhat H, Sosnovik DE. Diffusion Tractography of the Entire Left Ventricle by Using Free-breathing Accelerated Simultaneous Multisection Imaging. Radiology 2017;282(3):850-856.
Figures