1072
Noninvasive Assessment of Cerebral Collaterals with 3D Multi-inversion Time Arterial Spin Labeling in Ischemic Stroke: Comparison with DSA1Radiology, Tianjin Huanhu Hospital, Tianjin, China, 2Radiology, Liaocheng People’s Hospital, Liaocheng, China, 3Siemens Healthcare, Erlangen, Germany, 4MR Collaboration, Siemens Healthcare Ltd, Beijing, China
Synopsis
This study proposed a new method that can directly visualize and assess the collateral status by post-processing multiphase perfusion-weighted images (PWI) generated by multi-inversion time arterial spin labeling (mTI-ASL), and evaluate its performance by comparison with digital subtraction angiography (DSA) in patients with ischemic stroke. Comparison of the results of 28 patients showed that the collateral status assessed by the 3D mTI-ASL grading system was greatly consistent (kappa coefficient k = 0.854) with DSA. This technique is promising for the noninvasive assessment of the collateral status in stroke patients.
Introduction
Rapid and precise evaluation of the cerebral collateral circulation is vital for refining the therapeutic strategy in ischemic stroke1,2. Multi-inversion time arterial spin labeling (mTI-ASL) is an advanced technique that can noninvasively assess the cerebral hemodynamics by simultaneously measuring multiple parameters such as cerebral blood flow (CBF) and bolus arrival time (BAT).3Some studies have investigated the feasibility of using CBF and BAT to assess the collateral status by exploring their correlation. However, the clinical utility of multiphase perfusion-weighted images (PWI) generated by mTI-ASL, which may reflect the dynamics of intracranial blood flow, have not been investigated. This study aimed to develop a method that can directly assess the collateral status by post-processing of the multiphase PWI generated by mTI-ASL and evaluate its performance by comparing it with digital subtraction angiography (DSA) in patients with ischemic stroke.
Methods
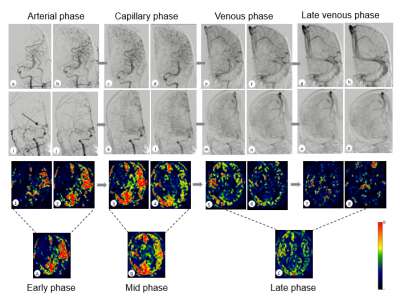
Twenty-eight patients (age, 58.0 ± 11.8 years; 22 males) with unilateral internal carotid artery occlusion (ICA) or middle cerebral artery (MCA) occlusion were prospectively enrolled. Informed consent was obtained from each subject. All patients were scanned on a 3T MAGNETOM Skyra scanner (Siemens Healthcare, Erlangen, Germany) with a 20-channel head coil. The mTI-ASL imaging was performed using a prototype sequence with the following parameters: 3D GRASE imaging with FAIRQ2TIPS labeling; TR/TE= 4600/22 ms; slice thickness = 4 mm; slices = 20; bolus duration = 700 ms; 16 TIs with TI ranging from 480 to 4080 ms, and TA= 5:09 mins including an M0 scan. All the patients also underwent a comprehensive DSA.Post-processing was completed using SPM12 (www.fil.ion.ucl.ac.uk/spm/software/Spm12). Before processing, 16 PWI images acquired by ASL were motion-corrected. In post-processing, the proposed method divided the 16 motion-corrected PWI images into three consecutive groups (5, 5, and 6 PWI images) and summed the images in each group separately to obtain three phasic images, with the early phase corresponding to the arterial phase in DSA, the middle phase corresponding to capillary phase in DSA, and the late phase corresponding to the venous phase and late venous phase in DSA. The obtained three phase images after post-processing, namely, the collateral flow map based on mTI-ASL, were used to assess the collateral status.
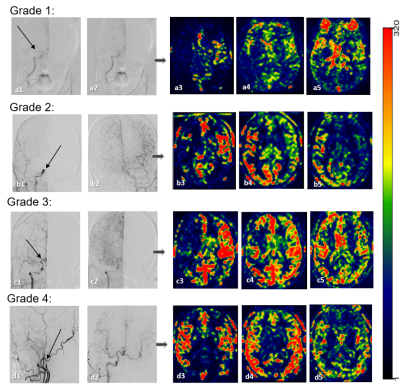
By referring to the ASTIN/SIR criteria for DSA, the collateral scoring criteria based on mTI-ASL were defined as follows: 0: no collateral perfusion to the MCA territory on the affected side; 1: slow collaterals (visible in the middle or late phase) to the MCA territory with persistence of the perfusion defects part; 2: rapid collaterals (visible in the early-to-middle phase) to the MCA territory with persistent perfusion defects; 3: slow but complete collateral perfusion visible in the MCA territory; and 4: rapid and complete collateral perfusion to the MCA territory.
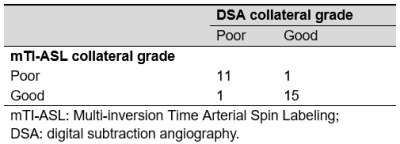
Two neuroradiologists independently assessed the collateral status based on DSA and mTI-ASL criteria with knowledge of symptomatic side and site of occlusion. Grade 0 - 2 was designated as poor collaterals and grade 3 - 4 as good collaterals. The agreement between the two observers for DSA- and ASL-based collateral grade, the consistency between 3D mTI-ASL, and DSA final grades were determined using kappa statistics.
Results
Among the 28 enrolled patients, 16 were diagnosed with ICA occlusion and 12 with MCA occlusion. The collateral flow status in a representative patient that was evaluated with DSA and mTI-ASL is demonstrated in Figure 1. Figure 2 shows the typical cases of the collateral grades scored by DSA and ASL. The inter-observer agreement for DSA and 3D mTI-ASL were 0.856 and 0.849, respectively. Table 1 shows the distribution of the collateral grade according to these two different modalities. In the DSA collateral grade system, 12 patients showed poor collaterals and 16 patients showed good collaterals, whereas 12 patients showed poor collaterals and 16 patients showed good collaterals in the mTI-ASL grading system. The consistency between the two methods was excellent (к = 0.854).Discussion & Conclusion
In ischemic stroke, DSA remains the reference standard for assessment of the intracranial collateral flow. A previous study also demonstrated the feasibility of using multiphase perfusion computed tomography (MPCT) to assess the collateral flow in acute stroke patients4. However, both methods are invasive and require ionizing radiation and potentially toxic exogenous contrast agents. Our study showed that the multiphase PWI images generated by 3D mTI-ASL can be used to directly visualize and assess the collateral status with excellent inter-observer agreement. The collateral status assessed by DSA and the proposed method showed high consistency, suggesting that our method may act as a promising tool to directly provide valuable collateral flow information for personalized treatment of ischemic stroke disease.Acknowledgements
This work was supported by the National Key Research and Development Program of China (No.2018YFC1312000).References
[1] Liebeskind, D. S. (2003). "Collateral circulation." Stroke 34(9): 2279-2284.
[2] Bang, O. Y., et al. (2011). "Collateral flow predicts response to endovascular therapy for acute ischemic stroke." Stroke 42(3): 693-699.
[3] Zhang, Jinge et al. “Comparative study of MR mTI-ASL and DSC-PWI in evaluating cerebral hemodynamics of patients with Moyamoya disease.” Medicine vol. 97,41 (2018): e12768.
[4] Kim, S. J., et al. (2012). "Multiphasic perfusion computed tomography as a predictor of collateral flow in acute ischemic stroke: comparison with digital subtraction angiography." Eur Neurol 67(4): 252-255
Figures