1067
Association of conventional vascular risk factors with asymptomatic and symptomatic intracranial atherosclerosis1Center for Brain Disorders Research, Capital Medical University and Beijing Institute of Brain Disorders, Beijing, China, 2Center for Biomedical Imaging Research, Department of Biomedical Engineering, Tsinghua University School of Medicine, Beijing, China, 3Department of Neurology, Beijing Tiantan Hospital, Capital Medical University; China National Clinical Research Center for Neurological Diseases, Beijing, China, 4Department of radiology, Sun Yat-sen Memorial hospital, Sun Yat-sen University, Beijing, China
Synopsis
This study investigated the association of vascular risk factors with asymptomatic and symptomatic ICAD using MR vascular wall imaging. Compared with controls, there was a positive association between hypertension and asymptomatic ICAD; and a positive association of hypertension, LDL, and diabetes and an inverse association of HDL with symptomatic ICAD (all p<0.05). Compared to asymptomatic ICAD, there was an inverse association between hyperlipidemia and symptomatic ICAD (p<0.001). We found that hypertension was a risk factor of asymptomatic ICAD and hypertension, diabetes and higher LDL were risk factors for symptomatic ICAD, whereas HDL was inversely associated with symptomatic ICAD.
Introduction
As one of the most common causes of ischemic stroke worldwide, intracranial atherosclerosis (ICAD) accounts for about 30%–50% of ischemic stroke or transient ischemic attacks (TIA) in Asia1-2. The vascular risk factors of ICAD included modifiable risk factors such as hypertension, diabetes, smoking and non-modifiable risk factors such as age, male sex, history of stroke3. Previous study reported that hypertension, higher low-density lipoprotein (LDL), and diabetes were associated with increased odds of ICAD, whereas higher levels of high-density lipoprotein (HDL) was associated with decreased odds of ICAD4-5. However, their specific impact on the occurrence of ICAD or symptom is poorly understood. The study sought to compare the conventional vascular risk factor among asymptomatic ICAD, symptomatic ICAD and controls using three-dimensional (3D) magnetic resonance (MR) vessel wall imaging.Methods
Study sample: One hundred and four symptomatic ICAD subjects (mean age, 57.2 ± 11.2 years; 67 males), 55 asymptomatic ICAD subjects (mean age, 70.6 ± 8.4 years; 24 males) and 430 controls without symptoms and ICAD (mean age, 58.5 ± 13.5 years; 158 males) were recruited. The study protocol was approved by local institutional review board and written consent form was obtained from each subject. Clinical information collection: Clinical information including age, gender, and conventional vascular risk factors (body mass index [BMI], smoking, drinking, hypertension, HDL, LDL, total cholesterol [TC], triglycerides [TG], diabetes, history of coronary heart disease [CHD], history of TIA, history of stroke and the National Institutes of Health Stroke Scale [NIHSS]) were collected from medical record. MR imaging: The MR imaging was conducted on 3.0T Philips or Siemens MR scanner with 8- or 36-channel phased array head coil or 16-channel neurovascular coil. A standardized imaging protocol includes T1 volumetric isotropic turbo spin echo acquisition (T1-VISTA) at Philips MR platform or T1 sampling perfection with application‐optimized contrast using different flip angle evolutions (T1-SPACE) sequence at Siemens MR platform. The T1-VISTA / SPACE imaging sequence was acquired using the following parameters: fast spin echo sequence / turbo spin echo, repetition time 800 / 900 ms, echo time 19 / 21 / 24 ms, field of view 200×181×45 / 200×180×40 / 158×158×158 mm³, matrix 332×300×150 / 332×332×133 / 256×256×246, thickness 0.6 mm, and scan time 7min1sec / 6min18sec / 8min6sec. Image analysis: The vessel wall images of intracranial arteries were interpreted by two experienced radiologists with consensus blinded to all clinical information. Intracranial atherosclerotic plaque is defined as eccentric wall thickening on MR vessel wall images. Presence or absence of atherosclerotic plaque at each vascular bed of intracranial arteries was determined. For each subject, if there was an atherosclerotic plaque in any vascular bed, this subject will be identified to have atherosclerotic plaque. Statistical analysis: Clinical characteristics were compared with One-way ANOVA and Tukey’s studentized range testing for continuous variables and Chi-square analysis or Fisher’s exact testing for categorical variables among three groups, as appropriate. A multivariate logistic regression was used to adjust for age, gender, and all vascular risk factors to test the association between outcome variable (3 groups: symptomatic ICAD, asymptomatic ICAD and controls) and each vascular risk factor. Two-tailed P-values <0.05 were considered statistically significant.Results
Comparison of vascular risk factors among three groups are shown in Table 1. There were significant differences in age, gender and vascular risk factors, except LDL, TG and prevalence of history of TIA among the three groups. Regression analysis for differences of vascular risk factors between symptomatic ICAD, asymptomatic ICAD and controls are shown in Table 2. When age, gender and all vascular risk factors were included in the multivariate model, compared with controls, there was a significant positive association between hypertension (OR: 2.50, 95% CI: 1.21-5.12, p = 0.013) and asymptomatic ICAD. In addition, there was a positive association of hypertension (OR: 8.36, 95% CI: 4.24-16.51, p <0.001), LDL (OR: 1.86, 95% CI: 1.02-3.41, p = 0.042), and diabetes (OR: 4.04, 95% CI: 2.14-7.62, p <0.001) and an inverse association of HDL (OR: 0.04, 95% CI: 0.01-0.14, p <0.001) with symptomatic ICAD. Moreover, compared to asymptomatic ICAD, there was a significant inverse association between hyperlipidemia (OR: 0.01, 95% CI: 0.001-0.12, p <0.001) and symptomatic ICAD.Discussion and Conclusion
Compared with controls, ICAD subjects were more frequently hypertensive, and symptomatic ICAD were more frequently hypertensive and diabetic and had a higher LDL, whereas HDL was inversely associated with symptomatic ICAD. This may explain the increased intracranial atherosclerotic plaques in asymptomatic subjects and the cause of symptoms of ICAD subjects. Therefore, effective control of hypertension, diabetes, and LDL may reduce the occurrence of symptomatic ICAD.Acknowledgements
None.References
1. Qureshi AI, Caplan LR. Intracranial atherosclerosis. Lancet. 2014;383(9921):984-998.
2. López-Cancio E, Galán A, Dorado L, et al. Biological signatures of asymptomatic extra- and intracranial atherosclerosis: the Barcelona-AsIA (Asymptomatic Intracranial Atherosclerosis) study. Stroke. 2012;43(10):2712-2719.
3. Banerjee C, Chimowitz MI. Stroke Caused by Atherosclerosis of the Major Intracranial Arteries. Circ Res. 2017;120(3):502-513.
4. Suri MF, Qiao Y, Ma X, et al. Prevalence of Intracranial Atherosclerotic Stenosis Using High-Resolution Magnetic Resonance Angiography in the General Population: The Atherosclerosis Risk in Communities Study. Stroke. 2016; 47(5):1187-1193.
5. Arenillas JF, Molina CA, Chacón P, et al. High lipoprotein (a), diabetes, and the extent of symptomatic intracranial atherosclerosis. Neurology. 2004;63(1):27-32.
Figures

Table 1. Comparison of vascular risk factors.
ICAD, intracranial atherosclerosis; HDL, high density lipoprotein; LDL, low-density lipoprotein TC, total cholesterol; TG, triglycerides; CHD, coronary heart disease; TIA, transient ischemic attacks; NIHSS, National Institutes of Health Stroke Scale.
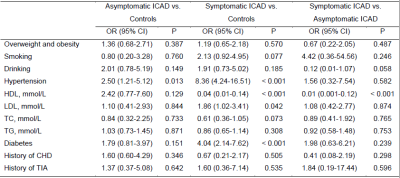
Table 2. Regression analysis for differences of vascular risk factors.
ICAD, intracranial atherosclerosis; HDL, high density lipoprotein; LDL, low-density lipoprotein TC, total cholesterol; TG, triglycerides; CHD, coronary heart disease; TIA, transient ischemic attacks.