1066
Accuracy of 3D High-Resolution Vessel Wall Imaging in Evaluating Internal Carotid and Intracranial Arterial Stenotic Lesions1Tianjin Medical University NanKai Hospital, Tianjin, China, 2Department of Radiology, Tianjin Huanhu Hospital, Tianjin, China, 3Department of Radiology, Tianjin First Central Hospital, Tianjin, China, 4siemens-healthineers, Tianjin, China
Synopsis
This study compared high-resolution vessel wall imaging (HR-VWI) and time-of-flight magnetic resonance angiography (TOF-MRA) for evaluation of stenosis using digital subtraction angiography (DSA) as the criterion standard. Compared with TOF-MRA, HR-VWI produced results that more closely agreed with DSA, showed better reproducibility and accuracy with smaller variance, and provided additional information on vessel wall pathology. HR-VWI may therefore be useful as an adjunct to DSA to diagnose stenosis and evaluate changes in intracranial vessel walls.
INTRODUCTION
In patients with stroke-like symptoms, intracranial atherosclerotic disease is the most frequent cause of vascular stenosis. However, the predominant vascular imaging modalities, such as digital subtraction angiography (DSA) and magnetic resonance angiography (MRA), only display luminal narrowing and are unable to provide information on the underlying pathology within the vessel wall. As a useful adjunct to conventional imaging methods, intracranial high-resolution vessel wall imaging (HR-VWI) may help diagnose the etiology of intracranial arterial narrowing 1. We hypothesized that HR-VWI would be more accurate than time-of-flight MRA (TOF-MRA) in evaluating different degrees of stenosis in intracranial artery disease (ICAD) using DSA as the criterion standard. This study was conducted to evaluate the consistency and accuracy of HR-VWI compared to TOF-MRA and 3D-DSA in assessing stenosis of different arterial segments, stenotic degrees, and pathological etiologies.METHODS
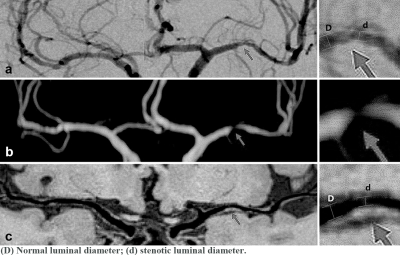
In this retrospective study, one hundred forty-eight patients with available HR-VWI, TOF-MRA, and DSA images were recruited. 3D-DSA was adopted as the gold standard for stenotic degree criteria. The MRI data were collected on a 3T system (MAGNETOM Prisma, Siemens Healthcare, Erlangen, Germany) with a standard 64-channel head/neck coil. HR-VWI was acquired using an inversion-recovery sampling perfection with application-optimized contrasts using different flip angle evolution (IR-SPACE) sequence with the following parameters: TR (repetition time) = 900 ms; TE (echo time) = 15 ms; 240 slices with a slice thickness of 0.60 mm; voxel size = 0.60×0.60×0.60 mm3; field of view = 240×87.5 mm2; acquisition time = 7 minutes 57s.2 TOF-MRA was performed with the following parameters: TR = 21 ms; TE = 3.42 ms; slice thickness = 0.90 mm; flip angle = 20°; field of view = 240×87.5 mm2; and acquisition time = 6 minutes 9 seconds. All assessments were separately rated by two radiologists and re-rated with a time interval of 2 weeks to minimize recall bias. The degree of stenosis in the internal carotid and intracranial arteries was assessed with the method used in the Warfarin-Aspirin Symptomatic Intracranial Disease (WASID) trial by measuring the diameter of the residual lumen at the maximal narrowing site, using the formula [1 - (diameter of stenosis/diameter of normal) / 100].3 The arterial luminal diameter distal or proximal to the maximal narrowing site was used as the normal value (Fig. 1). The degree of stenosis was classified into 3 groups: <50% (mild), 50% - 70% (moderate), and >70% (severe).4 Inter-observer agreement was assessed by interclass correlation coefficient (ICC). Bland-Altman plots and mountain plots were used to illustrate the concordance of HR-VWI and TOF-MRA, compared with DSA separately. The concordance correlation coefficient (CCC) was calculated to reflect the precision and accuracy of each method compared with DSA results. MedCalc (Version 18.1.1.0; MedCalc Software, Mariakerke, Belgium) was used for these analyses.5 P< 0.05 was considered statistically significant.RESULTS
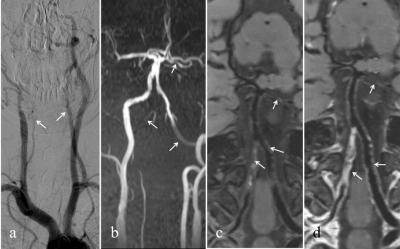
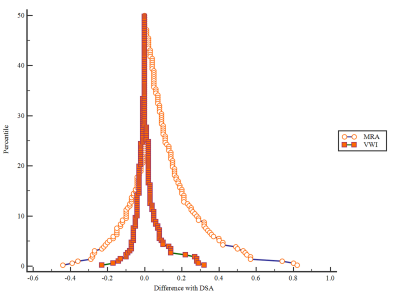
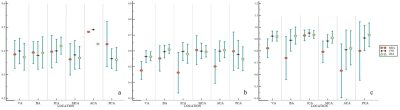
A total of 250 stenotic lesions from 106 individuals were analyzed; typical images are displayed in Fig. 2. HR-VWI showed better inter-observer reproducibility in the subgroups (mild, K=0.88; moderate, K=0.95; severe, K=1.00) than TOF-MRA (mild, K=0.78; moderate, K=0.93; severe, K=0.90). HR-VWI also showed better agreement with DSA than did TOF-MRA (ICC: HR-VWI=0.97; TOF-MRA=0.74) (Fig. 3). HR-VWI showed a higher degree of concordance with DSA (CCC=0.97) than did TOF-MRA (CCC=0.74) (Figs. 4 and 5). Additionally, the inter-observer reproducibility for any stenosis degree was higher for HR-VWI than for TOF-MRA (ICC: HR-VWI=1.00; TOF-MRA=0.98).DISCUSSION
HR-VWI demonstrated greater accuracy than TOF-MRA, as well as closer agreement with DSA in evaluating cervical and intracranial arterial stenosis. HR-VWI performed better in distal small vessels, provided more information on arterial abnormalities (including plaque and luminal thrombosis) and detected arterial stenosis with high reproducibility.5, 6 In particular, the ability of HR-VWI to assess the pathology of vessel walls may be valuable for clinical management. Additionally, HR-VWI is noninvasive and provides the further advantages of convenient examination, no use of X-ray, and rapid imaging.CONCLUSION
We conclude that HR-VWI is as accurate as DSA for the evaluation of intracranial artery stenosis and additionally can provide evidence of the underlying causative pathogenesis. HR-VWI is therefore a promising method for the diagnosis and management of stenosis of the carotid and intracranial arteries.Acknowledgements
This work was supported by Natural Science Foundation of China (NSFC) (grant numbers 81871342).References
1. Zhao DL, Li C, Chen XH, et al. Reproducibility of 3.0T High-Resolution Magnetic Resonance Imaging for the Identification and Quantification of Middle Cerebral Arterial Atherosclerotic Plaques. J Stroke Cerebrovasc Dis 2019;28:1824-1831.
2. Yang Q, Deng Z, Bi X, et al. Whole-brain vessel wall MRI: A parameter tune-up solution to improve the scan efficiency of three-dimensional variable flip-angle turbo spin-echo. J Magn Reson Imaging 2017;46:751-757.
3. Lee JN, Chung MS, Jung SC, et al. Comparison of High-Resolution MR Imaging and Digital Subtraction Angiography for the Characterization and Diagnosis of Intracranial Artery Disease. Am J Neuroradiol 2016;37:2245-2250.
4. Teng Z, Peng W, Zhan Q, et al. An assessment on the incremental value of high-resolution magnetic resonance imaging to identify culprit plaques in atherosclerotic disease of the middle cerebral artery. Eur Radiol 2016;26:2206-2214.
5. van der Palen RLF, Roest AAW, van den Boogaard PJ, de Roos A, Blom NA, Westenberg JJM. Scan-rescan reproducibility of segmental aortic wall shear stress as assessed by phase-specific segmentation with 4D flow MRI in healthy volunteers. MAGMA 2018;31:653-663.
6. Obusez EC, Hui F, Hajj-Ali RA, et al. High-resolution MRI vessel wall imaging: spatial and temporal patterns of reversible cerebral vasoconstriction syndrome and central nervous system vasculitis. AJNR Am J Neuroradiol 2014;35:1527-1532.
Figures