1065
Serial MR Vessel Wall Imaging Reveals Medical Treatment Response of Symptomatic Intracranial Atherosclerotic Plaque1Cedars-Sinai Medical Center, Los Angeles, CA, United States, 2Tianjin First Central Hospital, Tianjin, China, 3Beijing Chaoyang Hospital, Beijing, China, 4Tianjin Huanhu Hospital, Tianjin, China, 5University of California, Los Angeles, Los Angeles, CA, United States, 6Beijing Xuanwu Hospital, Beijing, China
Synopsis
Ischemic stroke is a leading cause of disability and death, also has a high recurrence rate. Serial magnetic resonance vessel wall imaging (MR-VWI) was used to quantify the morphological changes of intracranial atherosclerotic plaque during the medical treatment of ischemic stroke patients. Changes of quantitative plaque features were compared between patients with different clinical outcomes. Our study showed an increasing trend in most progression patients. Maximum wall thickness, pre-contrast plaque-wall contrast ratio
Introduction
Intracranial atherosclerotic disease (ICAD) represents one of the most common reasons for ischemic stroke worldwide1. The rate of stroke recurrence is still 13% in the first year and as high as 35% in certain populations by two years despite intensive medical management2. Intuitively monitoring therapeutic response in stroke patients can be challenging due to lack of lesion-specific examination methods. We aimed to use serial magnetic resonance vessel wall imaging (MR-VWI) to quantify the morphological changes of culprit lesions in response to medical therapy in patients with symptomatic ICAD.Methods
We retrospectively enrolled 24 patients with ischemic stroke secondary to intracranial atherosclerosis (20 M, age 46.8 years ± 14.1) from our institutional MR-VWI database. The inclusion criteria are as follows: (1) baseline MR-VWI was performed within 8 weeks of stroke onset and follow-up MR-VWI was performed between 3-18 months after stroke onset; (2) a luminal stenosis of ≥50% within the ischemic territory, confirmed by MRA or CTA; (3) no extracranial stenosis (>50%) tandem to the intracranial stenosis. All scans were obtained on the same 3T system (Siemens, Erlangen, Germany) in each patient. The protocol included DWI, 3D TOF-MRA, pre- and post-contrast VWI. VWI was performed using a recently developed 3D whole-brain VWI sequence3 with following parameters: TR/TE = 900/15 ms; field of view = 170×210 mm2/170×170 mm2; voxel size = 0.55/0.53 mm isotropic; scan time = 8 minutes. Post-contrast VWI was acquired 5 minutes after a bolus injection of Gd-DTPA at a dose of 0.1 mmol/kg body weight. The morphological features of culprit plaques, including plaque volume, peak normalized wall index (pNWI), maximum wall thickness, stenosis degree, pre-contrast plaque-wall contrast ratio (CR), and post-contrast plaque enhancement ratio (ER), were quantified on MR-VWI. Patients with 18-month clinical follow-up were divided into progression and non-progression groups depending on whether major vascular events (stroke, TIA, death) occurred. A paired-sample two-tailed t-test was used for comparisons between two MR-VWI examinations. Values of p< 0.05 were considered statistically significant.Results
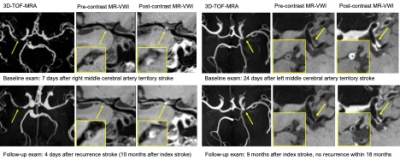
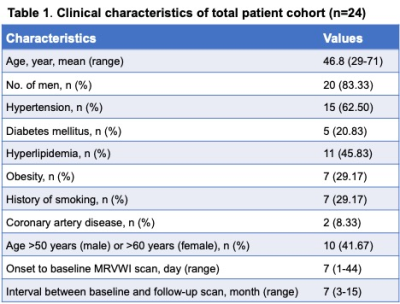
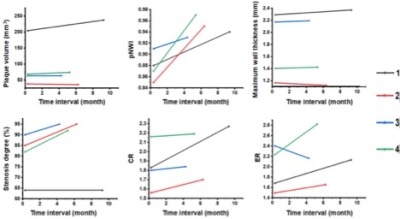
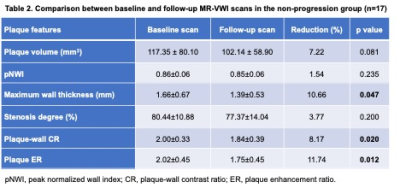
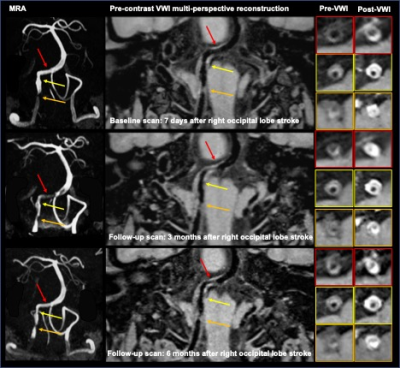
In the study, 21 patients had 18-month clinical follow-up out of 24 participants. Seventeen patients were categorized into the non-progression group and 4 into the progression group. Two representative cases in each group are shown in Figure 1. The baseline clinical characteristics of the 24 participants are shown in Table 1. Among the 24 patients, all interrogated plaque features exhibited changes during the course of medical therapy. Absolute percent changes were the largest in maximum wall thickness (20.93%±16.76%) and the least in pNWI (5.78%±3.85%). In addition, plaque volume (13.09%±11.23%), plaque-wall CR (12.44%±7.31%), and plaque ER (19.26%±11.17%) showed higher absolute percent changes than the stenosis degree (10.01%±8.58%). In the progression group, all 4 patients showed increases in pNWI, stenosis degree and CR; plaque volume, maximum wall thickness and ER increased in three patients (Figure 2). In the non-progression group, significant decreases were found in maximum wall thickness (-10.66%, p=0.047), plaque-wall CR (-8.17%, p=0.020) and plaque ER (-11.74%, p=0.012). Other features including pNWI (-1.54%, p=0.235), plaque volume (-7.22%, p=0.081) and stenosis degree (-3.77%, p=0.200) also decreased but no significance was reached (Table 2). A patient with two timepoints follow-up scans (3 months and 6 months) who had no recurrent events yet exhibited dramatic vessel wall changes despite medical therapy (Figure 3).Discussion
In patients who had recurrent vascular events within 18 months of stroke onset, we identified an upward trend among most of the plaque features that have been associated with acute cerebrovascular events. Conversely, all features showed a downward trend in patients who had no recurrent vascular events within the time window, which was particularly significant in maximum wall thickness, plaque-wall CR, and plaque ER. ICAD is a dynamic disease4. Hence, longitudinal assessments of plaque characteristics are likely more indicative of treatment response than a baseline assessment. Previous longitudinal studies of ICAD focused on the severity of luminal stenosis only5. In our work, several features demonstrated larger serial changes than stenosis degree did. Therefore, vessel wall-related plaque features and luminal stenosis are likely complementary to each other in the early detection of patients who are not responsive to prescribed medical therapy. We also found that worsening of ICAD lesions can occur in a short period of time despite medical treatment. These quantitative and lesion-specific markers may be more sensitive and specific than systemic serum biomarkers in terms of treatment response assessment. A prospective study with systematic control of medical management strategies and patient compliance and pre-defined follow-up timing would be warranted.Conclusion
Quantitative assessment of lesion-specific responses to medical therapy is clinically feasible with serial MR-VWI. The morphological changes of plaques over time may be useful for risk stratification in symptomatic ICAD patients on medical management.Acknowledgements
No acknowledgement found.References
1. Holmstedt CA, Turan TN, Chimowitz MI. Atherosclerotic intracranial arterial stenosis: risk factors, diagnosis, and treatment. Lancet Neurol 2013;12:1106-1114.
2. Derdeyn CP, Chimowitz MI, Lynn MJ, et al. Aggressive medical treatment with or without stenting in high-risk patients with intracranial artery stenosis (SAMMPRIS): the final results of a randomized trial. Lancet 2014;383:333-341.
3. Fan Z, Yang Q, Deng Z, et al. Whole-brain intracranial vessel wall imaging at 3 Tesla using cerebrospinal fluid-attenuated T1-weighted 3D turbo spin echo. Magn Reson Med 2017;77:1142-1150.
4. Famakin BM, Chimowitz MI, Lynn MJ, Stern BJ, George MG, Investigators WT. Causes and severity of ischemic stroke in patients with symptomatic intracranial arterial stenosis. Stroke 2009;40:1999-2003.
5. Leung TW, Wang L, Soo YO, et al. Evolution of intracranial atherosclerotic disease under modern medical therapy. Ann Neurol 2015;77:478-486.
Figures