1064
Atherosclerotic Plaques on Perforating Arteries Can be Detected by Vessel Wall Imaging at 7T in Patients with Single Subcortical Infarction1State Key Laboratory of Brain and Cognitive Science, Beijing MR Center for Brain Research, Institute of Biophysics, Chinese Academy of Sciences, Beijing, China, 2University of Chinese Academy of Sciences, Beijing, China, 3CAS Center for Excellence in Brain Science and Intelligence Technology, Beijing, China, 4Department of neurology, Beijing Tiantan Hospital, Capital Medical University, Beijing, China, 5China National Clinical Research Center for Neurological Diseases, Beijing Tiantan Hospital, Capital Medical University, Beijing, China, 6Siemens Shenzhen Magnetic Resonance Ltd., Shenzhen, China
Synopsis
Branch atheromatous disease (BAD) refers to small, deep brain infarcts that are predominantly caused by the occlusion of perforating arteries, which may lead to single subcortical infarction (SSI). However, there is no in-vivo radiological evidence of plaques in the perforating arteries due to their small caliber. In this study, we used high-resolution black-blood imaging at 7T to display the vessel wall of the anterior choroidal artery (AChA), and analyzed atherosclerotic plaques of AChA in patients with isolated infarcts on the posterior limb of internal capsule. The delineation of AChA plaques provides direct imaging evidence for the etiological diagnosis of BAD.
Introduction
Single subcortical infarction (SSI) may be caused by lipohyalinosis or branch atheromatous disease (BAD)1. BAD refers to small, deep brain infarcts that are predominantly caused by the occlusion of perforating arteries by atherosclerotic plaque, which is different from lipohyalinosis that is caused by lipohyalinotic degeneration of perforating arteries1. In previous studies, there was no radiographic depiction of the perforating artery plaques to reveal the pathological obstruction of the perforating artery. Imaging of the vessel wall pathology of BAD at 3T is challenging because of the small caliber of the perforating arteries. Recently, the development of 3D high-resolution vessel wall imaging (VWI)2 at 7T allowed for high-resolution delineation of the vessel wall of the perforating artery. In this study, the feasibility of using 7T VWI to display the wall of the anterior choroidal artery (AChA) was demonstrated. The atherosclerotic plaques on the AChA wall were analyzed in patients with isolated infarcts on the posterior limb of the internal capsule (PLIC).Methods
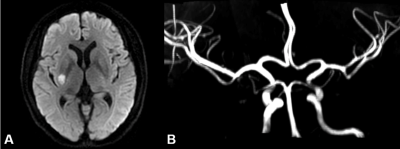
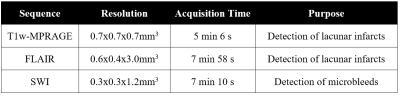
Fourteen patients from Tiantan Hospital with isolated infarcts in the territory supplied by the AChA (Fig. 1) were prospectively enrolled in the study. The patients were included for having lacunar infarctions in PLIC based on the finding of diffusion weighted imaging (DWI) at 3T. They all underwent scanning on a 7T MRI system (Siemens, Erlangen, Germany). A prototypical SPACE (sampling perfection with application-optimized contrasts using different flip-angle evolution) sequence was optimized for VWI. The following parameters were used: TR = 1200 ms, TE = 16 ms, voxel size = 0.40*0.40*0.40 mm3, FOV = 181*181*141 mm3, echo train length = 50, GRAPPA factor = 3, and TA = 10 min 29sec. High-resolution TOF-MRA covering the Circle of Willis was acquired with the following parameters: TR =15 ms, FA = 20°, TE = 4.3 ms, FOV = 180*135*47 mm3, TA = 7 min 34 s, and GRAPPA factor = 2. Other imaging sequences including T1-MPRAGE, FLAIR, and SWI were scanned for the diagnosis of structural lesions (Table. 1). The curved multi-planar reconstruction (curved-MPR) was obtained along the centerline from the end part of the internal carotid artery (ICA) to the AChA in Horos. Atherosclerotic plaque was defined as eccentric wall thickening with luminal stenosis identified in the curved-MPR of VWI, whereas the degree of stenosis was measured at the narrowest position of the lumen. The length of the AChA was also measured in the curved-MPR of TOF-MRA.Results
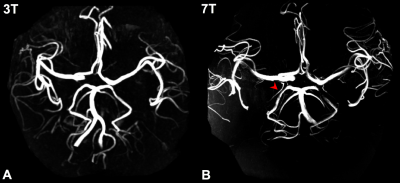
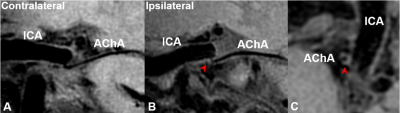
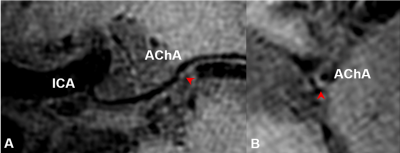
Two patients were excluded because of motion artifact, resulting in 12 patients in the final analysis. The length of the AChAs were 4.21 ± 0.96 cm measuring from their orifices on the ICA in 7T TOF-MRA, whereas they were almost invisible in TOF-MRA at 3T (Fig. 2). Twelve atherosclerotic plaques were found in AChA of all the patients. Nine of 12 plaques were found at the orifices of AChA, while only 3 atherosclerotic lesions were found in the middle section of AChA. The degree of stenosis was 54.6 ± 7.3% among the culprit AChAs. Fig. 3A showed the occlusion of the orifice and wall thickening of an AChA due to local thrombus in a patient, whereas no atherosclerotic lesions were found at the proximal segment of the AChA on the contralateral sides in Fig. 3B. Fig. 3C showed eccentric plaques in the transection of stenosis. Fig. 4 demonstrated an atherosclerotic lesion observed in the middle of AChA in another patient.Discussion
Atherosclerotic plaques could originate in the large artery and extend into the branch, or built up at the perforating artery. Our results showed that the orifices of the perforating branches could be blocked by atheromatous plaques, which accounts for most cases of PLIC infarctions (nine of 12 plaques were found at the orifices of AChA). Previous studies indicated that distal perforator disease was primarily caused by diffused lipohyalinosis degeneration of small vessels3. However, our findings suggested that some infarctions of PLIC can also be accounted by atheromatous plaques of perforating arteries, which was an important supplement to the pathological mechanisms of SSI4.The intrinsic black-blood effect of TSE (SPACE) enables superior suppression of blood flow with low velocity, making it possible to image the wall of perforating arteries5, such as the AChA. The delineation of AChA plaques provides direct imaging evidence for the etiological diagnosis of BAD. High-resolution VWI at 7T therefore allows a better understanding of the pathology of SSI.
In addition, AChA can be well displayed on 7T TOF-MRA due to higher SNR and higher resolution at ultra-high field. On the other hand, T1 relaxation becomes longer at 7T, which improves the flow-related enhancement in TOF-MRA and produces longer visible length in small arteries like the AChA.
Conclusion
The wall of the AChA can be visualized and analyzed on high-resolution VWI at 7T. The delineation of AChA plaques provides direct imaging evidence for the etiological diagnosis of BAD. High-resolution VWI at 7T may allow a better understanding of the pathology of SSI.Acknowledgements
This work was supported in part by the Beijing Municipal Natural Science Foundation (7184226), Young Elite Scientists Sponsorship Program by CAST (2017QNRC001), the grant of Ministry of Science and Technology of China (2017YFC1307904) and Beijing Municipal Natural Science Foundation(19G10046).References
1. Caplan LR. Intracranial branch atheromatous disease: a neglected, under- studied, and underused concept. Neurology. 1989; 39:1246–1250.
2. van der Kolk A G, Zwanenburg J J M, Brundel M, et al. Intracranial vessel wall imaging at 7.0-T MRI[J]. Stroke, 2011;42(9): 2478-2484.
3. Nah HW, Kang DW, Kwon SU, et al. Diversity of single small subcortical infarctions according to infarct location and parent artery disease: analysis of indicators for small vessel disease and atherosclerosis. Stroke. 2010; 41:2822–2827.
4. Nah H W, Kang D W, Kwon S U, et al. Diversity of single small subcortical infarctions according to infarct location and parent artery disease: analysis of indicators for small vessel disease and atherosclerosis[J]. Stroke. 2010;41(12): 2822-2827.
5. Zhang Z, Fan Z, Kong Q, et al. Visualization of the lenticulostriate arteries at 3T using black-blood T1-weighted intracranial vessel wall imaging: comparison with 7T TOF-MRA[J]. European radiology, 2019;29(3): 1452-1459.
Figures