1053
FLAIR-based estimation of the stroke onset time: a magnetic field dependent study1Department of Radiology, University of Pittsburgh, Pittsburgh, PA, United States
Synopsis
Stroke onset time is a prerequisite for thrombolytic treatment but is unknown in ~25% of acute ischemic stroke patients. A fluid-attenuated inversion recovery (FLAIR)-based MRI index (e.g., DWI-FLAIR mismatch) has been suggested as a surrogate to determine whether the stroke duration is within the treatment window. In this work, we showed that the time when a positive FLAIR contrast appears between ischemic and normal tissue increases with B0, and is dependent on the imaging parameters. Therefore, FLAIR-based studies of stroke onset should be designed or interpreted with care.
Introduction
The knowledge of stroke onset time is a prerequisite for thrombolytic treatment, but this information is unknown in ~25% of acute ischemic stroke patients. Recently, a fluid-attenuated inversion recovery (FLAIR)-based MRI index (e.g., DWI-FLAIR mismatch) has been suggested as a surrogate to determine whether the stroke duration is within the treatment window 1, but it is still unclear whether the efficacy of this index is dependent on the magnetic field strength. In this work, we aim to evaluate the field-dependence of the FLAIR signal in stroke with computer simulations and with experiments at a high field of 9.4 T.Methods
Simulations:The FLAIR signals were simulated for stroke durations between 0 to 24 hours and for B0 fields of 1.5, 3, 7 and 9.4 T. The T2 value of ischemic tissue was assumed to increase slowly due to vasogenic edema, with an initial rapid drop to the blood oxygenation level-dependent effect 2. The T1 value of the ischemic tissue was assumed to increase slowly, with an initial rise due to contribution from the cerebral blood flow 2,3.
Experiments:
Rats underwent permanent MCAO were scanned at 9.4 T. T1 and T2 maps were acquired up to 10 hours of occlusion to determine their rates of temporal changes. DWI and T2-FLAIR images were acquired for stroke durations between 1 to 5 h and at 24 h post occlusion. In typical T2-FLAIR studies, a long TR is chosen and the TI was selected to null the CSF signal. The echo time TE is usually selected to be close to the T2 of tissue water to optimize the signal to noise ratio (SNR). At 9.4 T, the T2 of normal tissue water is about 40 ms, and two echo times of 40 and 80 ms were acquired to compare their T2-FLAIR contrasts. Data in the ischemic core (defined by the ADC deficit regions) and the contralateral hemisphere were obtained for quantitative comparison.
Results and discussions
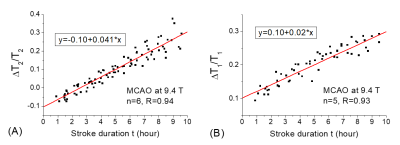
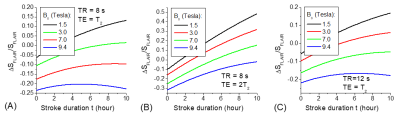
Linear fitting of the relative changes of T1 and T2 after stroke onset yields a slope of 2.0% and 4.1% per hour for T1 and T2, respectively (Fig. 1). There is an intercept of a ~10% increase of T1 and a ~10% decrease of T2 when extrapolating the data to the stroke onset (t=0), which is likely due to hemodynamic changes in the ischemic tissues. With typical T2-FLAIR imaging parameters, the simulated MRI signals initially drop below the baseline due to the rapid change of blood flow and oxygenation effects, and then slowly increase (Fig. 2). The rate of the increase is highly dependent on B0, but also on TR and TE. At a higher B0, there is a larger negative FLAIR contrast and slower increase over time. An increase in TR reduces the T1 effect, leading to a faster FLAIR signal increase. An increase of TE increases the T2 effect, also leading to faster FLAIR signal increase (but smaller baseline SNR).At 1.5 T, the zero-crossing time (when FLAIR signal intensity becomes higher than baseline) is less than 2-3 hours. At 3 and 7 T, the zero-crossing times are longer. At 9.4 T, the signal intensity is negative for most parameters used, i.e., no positive FLAIR contrast. This result is confirmed by our 9.4 T experimental data of MCAO rats. The FLAIR signal of the ischemic tissue (as identified by DWI) is always less than that of the contralateral normal tissue at the acute phase (1-5 h), i.e., negative FLAIR contrast, despite that both T1 and T2 already show significant increases at 4 h (Fig. 3). At 24 h post occlusion, the FLAIR contrast was still negative for TE = 40 ms and became close to 0 for TE = 80 ms (Fig. 4).
Conclusions
The time that a positive FLAIR contrast appears between ischemic and normal tissue increases with B0 and is dependent on the imaging parameters. This may explain previous reports that the efficacy of using the DWI-FLAIR mismatch as a biomarker for stroke onset estimation reduced at 3 T than 1.5 T 4,5. Thus, a FLAIR-based estimation of stroke onset should be designed or interpreted with care.Acknowledgements
Funding support from NIH: R01-NS100703.References
1. Thomalla G et al., Ann Neurol 2009; 65:724–732.
2. Calamante F et al., Magn Reson Med 1999; 41:479–485
3. Kettunen MI et al., Magn Reson Med 2000; 44:833–839.
4. Ebinger M et al., Stroke 2010; 41:250-255.
5. Emeriau S et al., Stroke 2013; 44:1647-1651.
Figures