1052
Comparison of Automated Cerebral Infarct Segmentation Techniques using DWI and FLAIR MRI1Biomedical Engineering, University at Buffalo, Buffalo, NY, United States, 2Canon Stroke and Vascular Research Center, University at Buffalo, Buffalo, NY, United States, 3Neurosurgery, University at Buffalo, Buffalo, NY, United States
Synopsis
FLAIR MRI has the potential to provide more accurate ground truth infarct labels compared with DWI for the purpose of software validation and determination of ischemic stroke patient eligibility for thrombectomy. Currently, accurate segmentation of infarct has hindered the use of FLAIR infarct labels due to skull and erroneous image intensity values being similar to those of infarct lesions. In this study, an automated segmentation technique was developed for segmentation of infarct tissue from FLAIR MRI and performance metrics comparing this method to manually segmented infarct (FLAIR Sorenson-Dice=0.8168, DWI Sorenson-Dice=0.7922) indicate this technique is non-inferior to the current standard (DWI).
Introduction
Throughout the world, 15 million people suffer from strokes each year. The majority of strokes are ischemic which occur due to an embolus blocking blood supply to the brain.1 This leads to formation of dead tissue known as infarct. Currently, diffusion weighted imaging (DWI) is the gold standard for located infarct tissue within acute ischemic stroke patients. This MRI method is reliant on diffusion of blood within the brain and, within regions of infarct, there is no diffusion leading to hyper-intensified regions in the image.2 A major issue with this method as the gold standard for infarct identification is hyper-intensified lesions have known to revert in cases of rapid reperfusion procedures.3 This indicates regions believe to be infarct are in fact a combination of infarct and penumbra (salvageable tissue deficient in blood flow). Due to this, fluid-attenuation inversion recovery MRI may supply more accurate indications of infarct tissue. This MRI method however, has supplied a more challenging issue in regards to infarct segmentation due to regions such as the skull having similar intensity values to infarct lesions.4 This study aims to assess the ability of a newly developed FLAIR MRI infarct segmentation technique in accurately isolating infarct regions to supply more reliable infarct ground truths.Methods
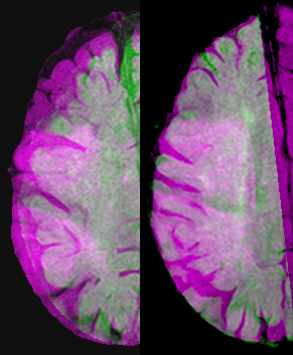
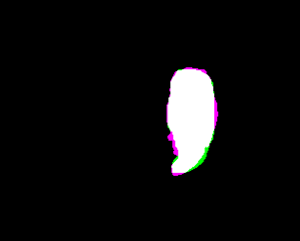
Data was retrospectively collected for 15 patients who suffered from acute ischemic strokes and underwent DWI and FLAIR MRI. Infarct segmentation was conducted for DWI imaging using a contralateral hemisphere comparison method previously reported. This method labels regions as infarct if their pixel intensity values are 162% greater in one hemisphere compared to the other.2 Additionally, manual segmentation of infarct regions was conducted from DWIs to compare the segmentation method to what we deemed as ground truth infarct labels. This comparison was conducted for future comparison with FLAIR MRI segmentation to determine if FLAIR MRI is a non-inferior method.Infarct segmentation was conducted within FLAIR MRIs using a contralateral hemisphere comparison method along with a comparison of average intensity values within a sampled portion of the FLAIR MRI. To conduct the contralateral hemisphere comparison, the FLAIR MRI was divided in half and the two hemisphere regions were overlapped. To eliminate potential errors from regions of the brain in one hemisphere laying outside the other hemisphere, geometric registration was conducted within MATLAB as indicated within Figure 1. Pixel values within each hemisphere were compared and values 120% greater in one hemisphere compared to the other were labeled as potential infarct regions. The hemisphere of the brain determined to not contain the stroke was then sampled using an automatically placed region of interest, and an average intensity from the region was taken. The regions previously labeled as potential infarct regions were compared with the average intensity value of the brain and if pixel intensities were 120% greater than this average value they were labeled as infarct. This image registration, average intensity and contralateral hemisphere comparison method aided in elimination of the skull and other hyper-intensified non-infarct regions being identified as infarct. Manual segmentation of infarct was performed within FLAIR MRI and compared with automated infarct regions. For all patients, accuracy, sensitivity, specificity, and Sorenson-Dice coefficients were calculated between automated and manual infarct segmentations (Figure 2). Additionally, comparisons of these values were conducted across DWI and FLAIR MRI.
Results
Table 1 indicates the average results for all 15 patients when comparing manual and automated segmentation techniques. Additionally, Table 1 compares overall results of this FLAIR MRI automated infarct segmentation technique with an implemented DWI infarct segmentation technique.Discussion
Analyzed data from the study indicates very high accuracy and specificity values for the DWI and FLAIR MRI infarct segmentation methods. This is expected since both of these metrics take into account the true negative values which encompass the majority of the MRI volume. The sensitivity and Sorenson-Dice coefficients meanwhile indicate moderate to high values for the DWI and FLAIR MRI automated infarct segmentation methods in comparison with manual segmentation of infarct. It is worth noting that the sensitivity and Sorenson-Dice coefficients for the FLAIR MRI segmentation are actually higher for these 15 patients compared to the DWI method. This indicates that the newly proposed FLAIR MRI infarct segmentation technique is a non-inferior method to segmenting infarct compared to DWI. This is of great significance since previously FLAIR MRI has posed significant problem in infarct segmentation.4 Additionally, these findings are significant since this method now supplies an alternative to providing more accurate cerebral infarct labels since FLAIR MRI infarct lesions are not known to revert in the manner DWI lesions are known to.Conclusion
In conclusion, this new infarct segmentation method can provide more accurate ground truth infarct labels since FLAIR MRI lesions are known to more accurately represent infarct tissue. These more accurate labels have the potential to be used for validation of other infarct location algorithms and determine potential eligibility for reperfusion procedures.Acknowledgements
The authors thank Ariana B. Allman and Alexander R. Podgorsak for their assistance in the completion of this project.References
1. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics—2017 update: a report from the American Heart Association. Circulation. 2017;135:e146.
2. Madai VI, Galinovic I, Grittner U, et al. DWI intensity values predict FLAIR lesions in acute ischemic stroke. PLoS One. 2014;9:e92295.
3. Inoue M, Mlynash M, Christensen S, et al. Early DWI reversal following endovascular reperfusion is typically transient in patients imaged 3-6 hours after onset. Stroke; a journal of cerebral circulation. 2014;45:1024.
4. Artzi M, Aizenstein O, Jonas-Kimchi T, et al. FLAIR lesion segmentation: application in patients with brain tumors and acute ischemic stroke. European journal of radiology. 2013;82:1512-1518.
Figures