0888
A fast T2 mapping protocol for prostate clinical applications using compressed sensing with low-rank and sparsity constraints1Philips Research, Hamburg, Germany
Synopsis
T2w-MRI plays an important role in prostate cancer providing information on the location/grade in diagnosis or surveillance. T2-mapping may provide objective characterization but is hampered by long acquisition time, which has been addressed by dedicated acceleration techniques (e.g. kt-T2 mapping). We investigate further acceleration of T2-mapping by prospective variable sub-sampling in the echo time domain, comparing regular or irregular patterns in combination with compressed sensing using low rank and sparsity constraints, towards a routine clinical T2 mapping protocol with increased volume coverage. Prostate and phantom T2-maps with 24 slices (1×1×3mm3 voxel) were acquired in 5½ minutes with promising map quality.
Introduction
T2w MRI plays an important role in prostate cancer (PCa) providing information on the location, volume and grade in diagnosis or active surveillance. However, the T2w hypointensity scored by the radiologist is hampered by low reproducibility of the acquisition. To address this, T2 mapping is explored for objective PCa characterization1. Multi-echo spin-echo based T2 mapping with sufficient organ coverage and spatial resolution (≤1mm in plane) is inherently slow. Previously, kt-T2 was proposed as a fast T2 mapping approach2, achieving a scan time of 5 minutes for 14 slices (40 mm FH coverage, 32 echoes) and was successfully applied in patient and reproducibility studies3. Based on regular k-space sub-sampling, shifted for each echo time, the dedicated kt-T2 reconstruction estimates missing data from adjacent echoes using a trained kernel. Here, we hypothesize that compressed sensing (CS) with low rank and sparsity constraints can provide higher acceleration in order to allow better coverage while maintaining map quality and acquisition time (5 min). Two approaches were investigated in phantom and prostate volunteer examinations: (1) Use a CS reconstruction on regularly sub-sampled data as in kt-T2; (2) Apply an irregular Poisson disk sampling (ky-echo) pattern to adapt the sub-sampling for CS reconstruction.Methods
Irregular (see Fig.1a) or regular sub-sampling patterns (Fig.1b) along the echo time dimension were implemented by introducing ky blip gradients during a fast multi-echo spin echo readout. The regular pattern was similar as in kT-T2 mapping2, and the irregular pattern used Poisson disk sampling in the ky-TE plane. 3 lines were fully sampled.Reconstruction used a fast low rank and sparsity regularization algorithm4, implemented in the MRI system SW, solving the following minimization problem for N echoes:
$$\underset{M}{\operatorname{argmin}} \left( \frac{1}{2} \| EM-P \|^2_2 + \lambda_1 \| W(M) \|_1 + \lambda_2 \| M \|_{*} \right)$$
Here, M is a matrix with N columns of vectorized echo images, P a matrix of N measured k-spaces, E the encoding matrix, including sub-sampling and coil sensitivity maps, $$$\lambda_1$$$ and $$$\lambda_2$$$ are regularization parameters (values chosen here 0.025 and 0.0015), W is the wavelet transform, $$$\| M \|_{*}$$$ is the nuclear norm of matrix M. T2 maps were computed from the multi-echo series using the standard MR system reconstruction (maximum likelihood estimation).
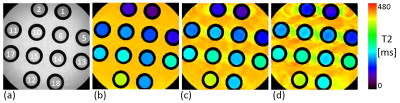
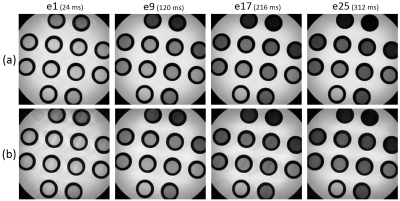
Experiments were performed on a 3T MRI system (Ingenia, Philips, NL) using a reference phantom (Eurospin-TO5, Diagnostic Sonar, GB, 12 samples T2=50…370ms, T1=220…1620ms, see Fig2.a) and volunteer examinations (n=3), with informed consent obtained. The following imaging parameters were used: FOV 160×160×72 mm3, voxel 1.0×1.0×3.0 mm3, reconstruction 0.7mm, 24 slices; acceleration R=11, TR = 4800ms, TEn = (24 + n*12) ms, α=90°, refocusing control αrefo,n={172°,132°,120°,120°,120°…}, B1max=8μT, whole body SAR < 1.7W/kg, scan duration 5½min. A reference T2 map was acquired for the phantom using identical parameters except for 2D single slice, SENSE R=2.4 (no CS) and a scan duration of 25min, as well as a T2w fast spin echo scan (voxel size 0.4×0.6×3.0 mm3, TR/TE=2780/110ms, CS-SENSE R=2, 2min46s).
Results
Figure 2 shows exemplary results from fast T2-mapping phantom tests. The reference Fig.2b is compared to the multi-slice fast acquisition with Poisson disk sampling Fig.2c and regular sampling pattern Fig.2d. Selected echo images are shown in Figure 3, (Fig.3a irregular, Fig.3b regular sampling). The irregular sampling shows consistent image quality (T2-maps and echo images) while the regular sampling pattern reveals residual foldover artifacts. Fitting the T2 values between reference and CS acquisition shows consistent linearity but some bias. For the irregular case: T2[c] = 0.965×T2[b] + 20.2ms (R = 0.9995). Regular sampling results are less consistent in terms of quantitative values and show a larger bias: T2[d] = 0.884×T2[b] + 46.2ms (R=0.9979). Figure 4 shows 6 selected adjacent slices from a prostate volunteer exam. T2-maps based on prospective irregular and regular sub-sampling are shown in Fig.4a and Fig.4b, respectively, using greyscale with T2=0…250ms. Fig.4c shows the same slices from a T2w reference scan. While the prostate is sharply depicted in the T2 maps for all slices in the irregular case, some foldover and slight blurring of the maps is apparent for the regular sampling case.Discussion
Quantitative T2 maps at the chosen high acceleration could be obtained in phantom and volunteer experiments with a promising quality and within a clinically relevant acquisition time by applying variable sub-sampling across echoes and CS reconstruction. The CS acceleration enables acquiring T2 maps with the same FH coverage (e.g. 24 slices, 72mm) as conventional T2w-MRI, avoiding the precise planning required in previous works to fit the prostate into the imaging volume. Regarding the consistency of quantitative values and the map quality (foldover artifacts), the irregular pattern was found superior to the regular sampling, given the same acquisition time and reconstruction parameters. With the chosen reconstruction parameters, the quantitative values show a bias of 20ms (irregular sampling), which is relevant for the short T2 times in prostate cancer (about 100ms). Further investigation is underway to reduce this bias. Using a larger number of echoes with shorter echo time (e.g. 40 echoes with ΔTE=9ms) further improvement of the T2 reconstruction stability can be expected.Acknowledgements
No acknowledgement found.References
1. Chatterjee A, Devaraj A, Mathew M, Szasz T, Antic T, Karczmar GS, Oto A. Performance of T2 Maps in the Detection of Prostate Cancer. Acad Radiol. 2019 Jan;26(1):15-21.
2. Liu W, Turkbey B, Sénégas J, Remmele S, Xu S, Kruecker J, Bernardo M, Wood BJ, Pinto PA, Choyke PL. Accelerated T2 mapping for characterization of prostate cancer. Magn Reson Med. 2011 May;65(5):1400-6.
3. van Houdt PJ, Agarwal HK, van Buuren LD, Heijmink SWTPJ, Haack S, van der Poel HG, Ghobadi G, Pos FJ, Peeters JM, Choyke PL, van der Heide UA. Performance of a fast and high-resolution multi-echo spin-echo sequence for prostate T2 mapping across multiple systems. Magn Reson Med. 2018 Mar;79(3):1586-1594.
4. J. Yao, Z. Xu, X. Huang, and J. Huang. An efficient algorithm for dynamic MRI using low-rank and total variation regularizations. Med. Image Anal., vol. 44, pp. 14–27, Feb. 2018.
Figures