0841
Pulmonary MR Imaging with Ultra-Short TE: Capability of Nodule Detection and Lung RADS Classification for Lung Cancer Screening1Radiology, Fujita Health University School of Medicine, Toyoake, Japan, 2Radiology, Kobe University Graduate School of Medicine, Kobe, Japan, 3Canon Medical Systems Corporation, Otawara, Japan, 4Diagnostic Radiology, Hyogo Cancer Center, Akashi, Japan
Synopsis
No report has been found to compare the capability of pulmonary MR imaging with UTE for nodule detection and Lung-RADS classification as compared with low-dose CT (LDCT) and standard-dose CT (SDCT). We hypothesized that pulmonary MR imaging with UTE has a similar potential to detect pulmonary nodules and evaluate Lung-RADS classification as well as LDCT and SDCT. The purpose of this study was to compare the capability of pulmonary MR imaging with UTE for lung nodule detection and evaluation of Lung-RADS classification with LDCT and SDCT.
Introduction
National Lung Cancer Screening Trail (NLST) reported 20% reduction in mortality with the use of low-dose computed tomography (LDCT) scan to screen high risk individuals. Therefore, major organizations including US Preventive Services Task Force has adopted LDCT for lung cancer screening in high risk populations. In addition, American College of Radiology has designed Lung-RADS as a quality assurance tool to standardize lung cancer screening CT reporting and management recommendations, reduce confusion in lung cancer screening CT interpretations, and facilitate outcome monitoring (1). Since 2016 (2-4), pulmonary MR imaging with ultrashort TE (UTE) less than 200ms has been suggested as having a potential to detect nodule, evaluate lung parenchymal abnormality and play as substitution to LDCT as well as standard-dose CT (SDCT). However, no report has been found to compare the capability of pulmonary MR imaging with UTE for nodule detection and Lung-RADS classification as compared with LDCT and SDCT. We hypothesized that pulmonary MR imaging with UTE has a similar potential to detect pulmonary nodules and evaluate Lung-RADS classification as well as LDCT and SDCT. The purpose of this study was to compare the capability of pulmonary MR imaging with UTE for lung nodule detection and evaluation of Lung-RADS classification with LDCT and SDCT.Materials and Methods
110 consecutive patients (64 males: mean age, 67 years and 46 females: mean age, 65 years) with suspected pulmonary nodules at near-by hospital were examined with pulmonary MR imaging with UTE at a 3T system (Vantage Titan 3T, Canon Medical Systems Corporation, Otawara, Japan) by respiratory-gated 3D radial UTE pulse sequence (TR 4.0ms/ TE 110-192μs, flip angle 5 degree, 1×1×1 mm3 voxel size), SDCT (270 mA) and LDCT (60 mA) at 64-detector row CTs (Aquilion 64, Canon Medical) and 320-detector row CTs (Aquilion ONE, Canon Medical). According to SDCT findings, all nodules were divided into solid and part-solid nodules and ground glass nodules. In each patient, probability of presence at each pulmonary nodule was assessed on all three methods by means of 5-point visual scoring system by two board certified chest radiologists. In addition, all nodules were classified based on Lung-RADS on each method by same radiologists. To compare nodule detection capability, Jackknife alternative free-response receiver operating characteristic (JAFROC) analysis were performed among all methods. Then, detection rates were also compared among three methods by McNemar’s test. To evaluate Lung-RADS classification capability, inter-observer agreement of each method was evaluated by kappa statistics with χ2 test. In addition, inter-method agreements were also assessed by kappa statistics with χ2 test were performed. A p value less than 0.05 was considered as significant in this study.Results
Representative case is shown in Figure 1, 2 and 3. Results of JAFROC analysis are shown in Figure 4. Figure of merit (FOM) of all methods based on consensus reading (MRI with UTE: FOM=0.89, LDCT: FOM=0.86, SDCT: FOM=0.89) had no significant differences (F=0.13, p=0.89). In addition, sensitivity (SE) and false-positive rate per case (FPR) of all methods (MR imaging with UTE: SE, 0.93, FPR, 0.55; LDCT; SE, 0.93, FPR, 0.68; SDCT: SE, 0.93, FPR, 0.62) had no significant difference (p>0.05). On Lung-RADS classification, interobserver agreement of each method was as follows: MR imaging with UTE: κ=0.92, p<0.0001; LDCT: κ=0.93, p<0.0001; and SDCT: κ=0.96, p<0.0001. When assessed inter-method agreements among all methods, inter-method agreements were also almost perfect (MR imaging with UTE vs. LDCT: κ=0.86, p<0.0001; MR imaging with UTE vs. SDCT: κ=0.87, p<0.0001; LDCT vs. SDCT: κ=0.95, p<0.0001).Conclusion
Pulmonary MR imaging with UTE is considered at least as valuable as LDCT and SDCT for lung nodule detection and Lung-RADS classification.Acknowledgements
Authors wish to thank Mr. Katsusuke Kyotani and Prof. Takamichi Murakami in Kobe University Hospital for their valuable contributions to this study.References
- American College of Radiology. Lung CT Screening Reporting and Data System (Lung-RADS). Accessed at www.acr.org/Quality-Safety/Resources/LungRADS on 12 October, 2019.
- Ohno Y, Koyama H, Yoshikawa T, et al. J Magn Reson Imaging. 2016; 43(2): 512-532.
- Ohno Y, Koyama H, Yoshikawa T, et al. Radiology. 2017; 284(2): 562-573.
- Wielpütz MO, Lee HY, Koyama H, et al. AJR Am J Roentgenol. 2018; 210(6): 1216-1225.
Figures

Figure 1. 57-year old female patient with ground-glass nodule in the right upper lobe.
All methods clearly demonstrate a ground-glass nodule in the right upper lobe. This case was assessed as Catogory 2 in Lung-RADS on each method.

Figure 2. 62-year old male patient with part-solid nodule in the right upper lobe.
All methods clearly demonstrate a part-solid nodule in the right upper lobe. This case was assessed as Catogory 4 in Lung-RADS on each method.

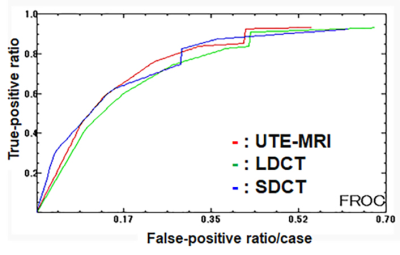
Figure 4. Results of JAFROC analysis.
There were no significant difference of figure of merit among all methods (F=0.13, p=0.89).